Opioid Itching Diagnostic Tool
Opioid Itching Assessment
This tool helps determine if your opioid-induced itching is most likely caused by histamine or nerve activation, and suggests the most effective treatment options based on your symptoms.
When you take an opioid for pain - whether it’s morphine after surgery or fentanyl during labor - you expect relief. You don’t expect to feel like fire ants are crawling under your skin. Yet, opioid-induced itching happens to up to 100% of people getting spinal morphine. It’s not an allergy. It’s not dry skin. It’s a direct effect of the drug itself, and it’s more common than most doctors admit.
Why Does Opioid Itching Happen?
For decades, doctors blamed histamine. The idea was simple: opioids like morphine and codeine trigger mast cells in the skin to dump histamine, just like an allergic reaction. That’s why antihistamines like diphenhydramine (Benadryl) were handed out like candy. But here’s the problem - they barely work. Recent research shows histamine is only part of the story. In fact, clinical doses of opioids don’t reliably release enough histamine to cause the itching most patients feel. The real culprit? Your nerves. Opioids activate mu opioid receptors (MOR) not just in the brain, but along nerve fibers in the spinal cord and skin. These receptors are packed tightly in areas like the face, chest, and arms - which is why itching hits there first. When activated, they send false itch signals straight to your brain. Think of it like a glitch in the system: the same drug that turns down pain signals accidentally turns up itch signals. A 2018 study in Nature Scientific Reports proved this by injecting a pure MOR activator (DAMGO) under the skin. Patients scratched. Then they gave a drug that blocks opioid receptors only in the skin - and the itching stopped. No histamine involved. Just nerves being tricked.The Histamine Debate: Still Relevant?
You’ll still hear some doctors say histamine is the cause. And yes, there’s some truth to it. Morphine and meperidine can cause mast cells to release histamine - especially at high doses or in people with sensitive skin. That’s why some patients get hives or redness along with the itch. But here’s the key difference: histamine-driven itching usually comes with visible signs - swelling, red bumps, flushing. Opioid-induced itching? Often it’s just a deep, crawling sensation with no rash. That’s the nerve-driven kind. And that’s what most patients experience. A 2023 review in the European Journal of Pain put it plainly: “The histamine hypothesis explains only a small fraction of cases.” If your itching has no rash, no swelling, and doesn’t respond to Benadryl, it’s not histamine. It’s your nerves.What Treatments Actually Work?
If antihistamines fail, what do you do? The answer isn’t more drugs - it’s smarter drugs. Naloxone - yes, the opioid overdose reversal drug - is surprisingly effective. At tiny doses (0.25 mcg/kg/min), it blocks opioid receptors in the skin without touching the ones in your spine that control pain. Studies show it cuts itching by 60-80%. And it doesn’t make your pain worse - if you dose it right. Nalbuphine is even better for many patients. It’s a mixed drug: it blocks mu receptors (so it stops itching) but activates kappa receptors (which calm nerves without causing sedation). At 5-10 mg IV, it works in under 5 minutes. Nurses in post-op units swear by it. One posted on AllNurses: “Nalbuphine 2mg IV - works faster than Benadryl, no drowsiness, patients sleep through it.” Butorphanol is another kappa agonist. In cesarean patients, it dropped itching scores from 8.2 to 2.1 on a 10-point scale. That’s not just relief - that’s life-changing. IV lidocaine (1.5 mg/kg) works in about 70% of cases. It numbs the nerves. But it’s not for everyone - you need to monitor heart rhythm. It’s a backup option. And here’s the kicker: timing matters. If you wait 30 minutes to treat the itch, it’s harder to stop. The sweet spot? Give the treatment within 5-10 minutes of the first scratch.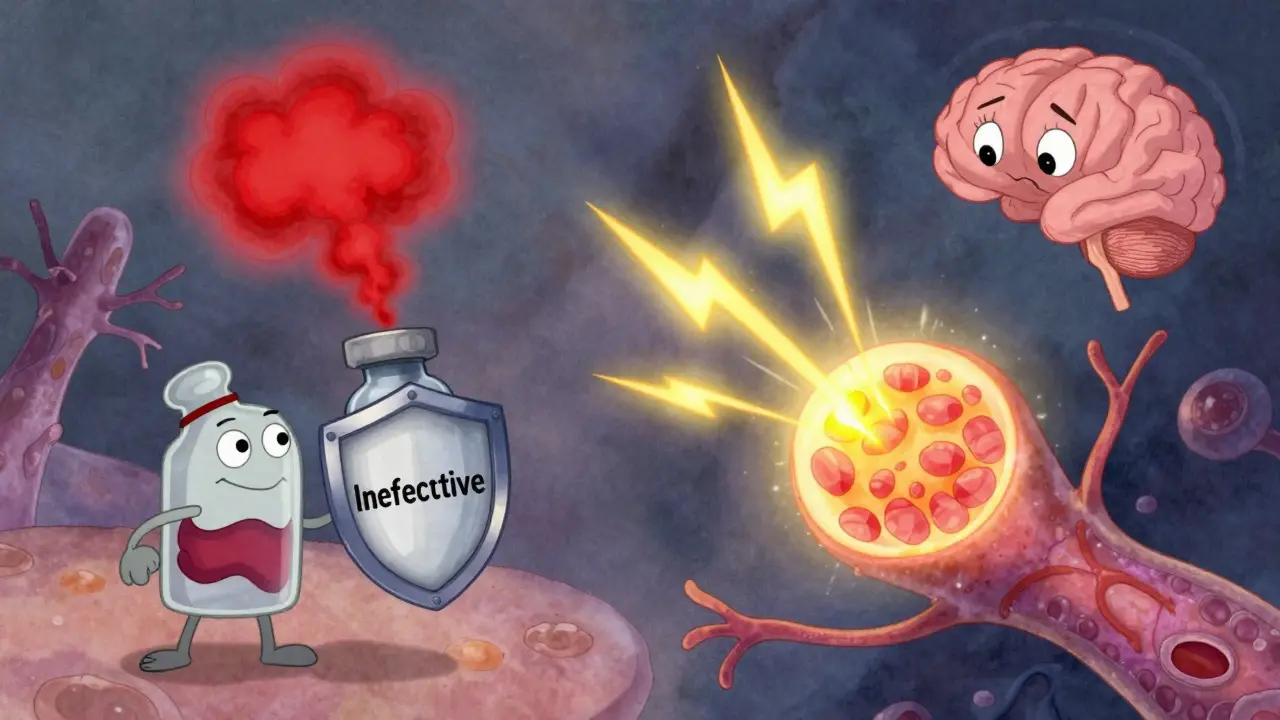
Why Do So Many Doctors Get It Wrong?
Because they’re taught the old story: histamine = itching = antihistamine. A 2019 study in Anesthesia & Analgesia found 32% of clinicians mistook opioid-induced itching for anaphylaxis. That’s dangerous. Some patients got epinephrine - a powerful drug meant for life-threatening allergies - when all they needed was a tiny dose of nalbuphine. Also, itching is often dismissed as “just a side effect.” But patients don’t see it that way. In postpartum forums, 78% of mothers said itching ruined their first hours with their newborn. One wrote: “I couldn’t hold my baby because I was scratching my face raw.” In chronic pain groups, 22% quit opioids entirely because of the itch. “I’d rather have pain than feel like fire ants are crawling under my skin 24/7,” said one user on ChronicPainSupport.org.What’s Coming Next?
The future of treating opioid itching is precision. New drugs like CR845 (difelikefalin) - a kappa agonist that doesn’t cross into the brain - are in Phase II trials. They reduce itching by 65% without drowsiness, low blood pressure, or pain relief interference. By 2028, experts predict 75% of major hospitals will use mu antagonist/kappa agonist combos as first-line treatment. That’s nalbuphine, butorphanol, or next-gen drugs - not antihistamines. Meanwhile, the FDA now requires opioid labels to include pruritus management guidelines. Hospitals like the University of Copenhagen have created “Pruritus First Response Algorithms” - step-by-step plans for nurses. Those hospitals saw a 40% drop in rescue meds.What Should You Do?
If you’re getting an opioid - especially via IV or spinal route - ask:- “What’s the plan if I start itching?”
- “Will you use nalbuphine or naloxone instead of Benadryl?”
- “Can we start treatment right away if I feel it?”
Practical Takeaways
- Itching after opioids? It’s likely not histamine - it’s nerve activation.
- Antihistamines like Benadryl work in only 20-30% of cases.
- Nalbuphine (5-10 mg IV) is the most effective single-agent treatment.
- Timing is everything: treat within 5-10 minutes of onset.
- Look for itching on the face, chest, arms - not the legs - that’s the nerve pattern.
- Redness or hives? That’s histamine. No rash? That’s neural.
- Don’t confuse this with an allergic reaction. Epinephrine won’t help.
Doctors are starting to catch up. But until they do, know the facts. You deserve pain relief - without the unbearable itch.

