Probiotics and Immunosuppressants: What You Need to Know
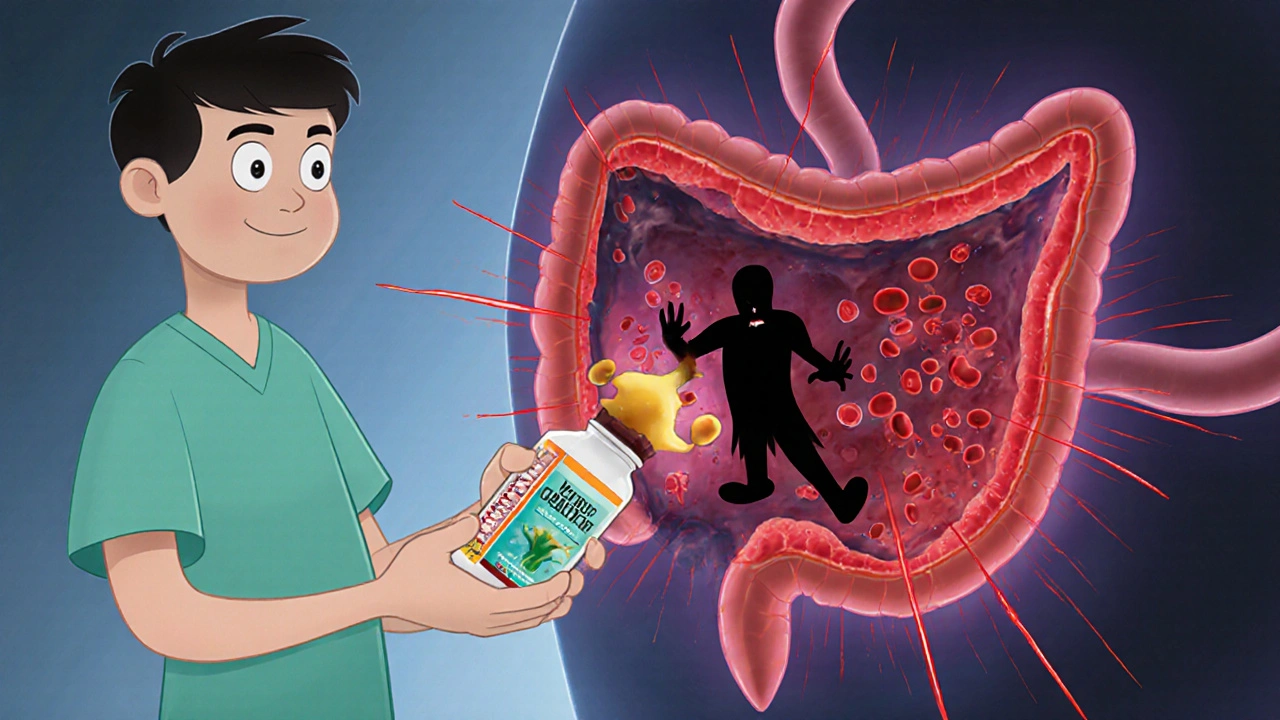
When you take immunosuppressants, drugs that lower your immune system’s activity to prevent organ rejection or control autoimmune diseases. Also known as immune inhibitors, they help manage conditions like Crohn’s disease, lupus, or after a transplant. But if you’re also using probiotics, live bacteria that support gut health and may help balance your microbiome. Often found in yogurt, kefir, or supplements, they’re meant to boost digestion and immunity. Here’s the catch: these two don’t always play nice together.
Immunosuppressants work by dialing down your body’s natural defenses. That’s good if your immune system is attacking your own tissues. But it also leaves you more vulnerable to infections. Probiotics, on the other hand, are living organisms. Even though they’re usually harmless, introducing them into a body with a suppressed immune system can be risky. There’s real evidence—like case reports from transplant centers—that probiotics have triggered bloodstream infections in people on strong immunosuppressants. It’s rare, but it happens. And if you’re on drugs like cyclosporine, tacrolimus, or azathioprine, your body isn’t fighting back the way it used to. So what seems like a harmless supplement might turn into a problem.
That doesn’t mean you have to ditch probiotics entirely. Many people on immunosuppressants still benefit from them—especially if they’re dealing with antibiotic-related diarrhea or gut inflammation. The key is choosing the right strain, the right dose, and talking to your doctor first. Not all probiotics are the same. Lactobacillus and Bifidobacterium strains are common, but some are safer than others in immunocompromised people. Your doctor might recommend a specific brand or avoid them altogether based on your meds and health history.
And it’s not just about the probiotics themselves. Your gut health affects how your body absorbs and reacts to immunosuppressants. If your microbiome is out of balance, your drug levels might fluctuate. That can mean your meds aren’t working right—or worse, they’re causing side effects. Some studies suggest that people with healthier gut bacteria respond better to these drugs. But again, that doesn’t mean popping a probiotic pill is the fix. It’s about long-term balance, not a quick fix.
You’ll also find posts here that dig into how other substances—like coffee, chocolate, or even herbal supplements—can interfere with medications. That’s because what you eat, drink, or take doesn’t exist in a vacuum. Your gut, your immune system, and your meds are all connected. That’s why the articles below cover everything from anticholinergic drugs and blood pressure meds to how acupuncture or yoga might support your overall care. They’re not random. They’re all pieces of the same puzzle: how your body responds to treatment, what you can control, and what you should avoid.
Below, you’ll find real-world comparisons, safety tips, and practical advice from people who’ve been there. Whether you’re on immunosuppressants and wondering if your probiotic is safe—or just trying to understand how your gut affects your meds—these posts give you the facts without the fluff. No guesswork. Just clear, direct info to help you make smarter choices.