Understanding Secondary Hyperparathyroidism
Before we dive into the connection between secondary hyperparathyroidism and osteoporosis, it's important to understand what secondary hyperparathyroidism is. This condition occurs when the parathyroid glands produce too much parathyroid hormone (PTH) in response to low levels of calcium in the blood. The primary function of PTH is to regulate calcium levels, so when there is a deficiency, the glands work overtime to bring the levels back up.
Secondary hyperparathyroidism is often caused by conditions that affect calcium absorption, such as chronic kidney disease, vitamin D deficiency, and certain medications. It is important to identify and address these underlying causes in order to effectively treat secondary hyperparathyroidism and prevent complications, such as osteoporosis.
Osteoporosis: A Common Bone Disease
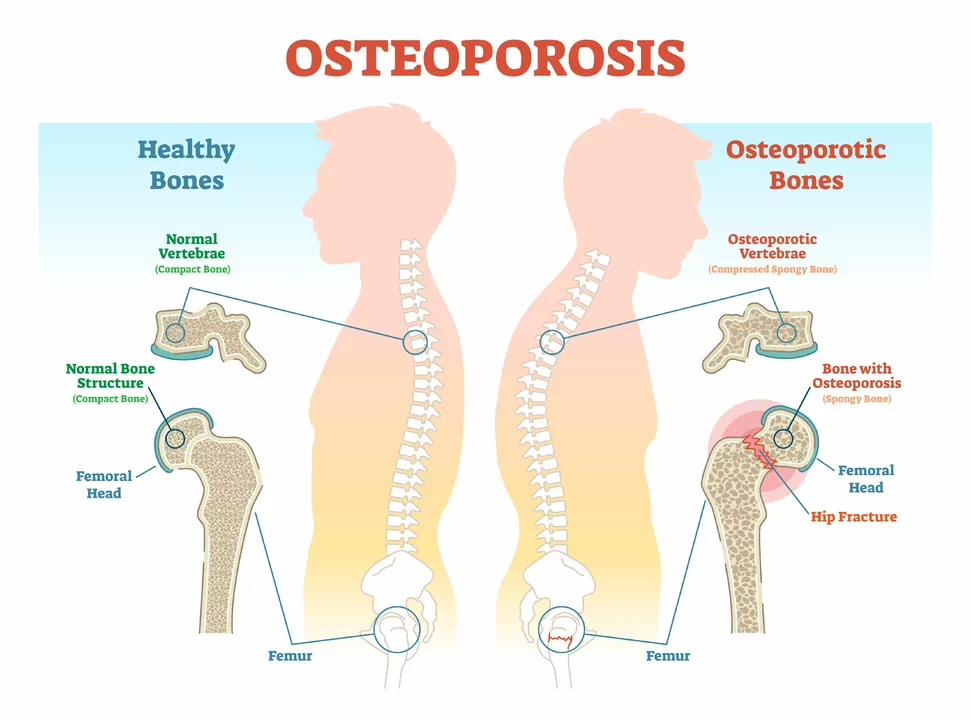
Osteoporosis is a common bone disease characterized by decreased bone density and increased risk of fractures. It affects millions of people worldwide, especially older adults and postmenopausal women. In osteoporosis, the rate of bone resorption (breaking down) exceeds the rate of bone formation, leading to weakened and brittle bones.
There are many factors that contribute to the development of osteoporosis, including age, genetics, hormonal changes, and lifestyle factors like diet and exercise. However, the connection between secondary hyperparathyroidism and osteoporosis is an important aspect to consider when discussing bone health.
How Secondary Hyperparathyroidism Affects Bone Density
As mentioned earlier, secondary hyperparathyroidism is characterized by an overproduction of PTH. One of the main effects of PTH on the body is to stimulate the release of calcium from the bones into the bloodstream. This process, known as bone resorption, is a normal part of bone remodeling. However, when PTH levels are chronically elevated due to secondary hyperparathyroidism, the rate of bone resorption increases significantly.
This excessive bone resorption leads to a decrease in bone density, which can eventually result in osteoporosis. In addition to increasing bone resorption, high PTH levels can also interfere with bone formation, further contributing to the weakening of bones.
Identifying the Link Between the Two Conditions
Research has shown a clear link between secondary hyperparathyroidism and osteoporosis. Studies have found that patients with secondary hyperparathyroidism have a higher prevalence of osteoporosis and an increased risk of fractures compared to those without the condition. This is likely due to the effects of excess PTH on bone remodeling, as described above.
Moreover, treating the underlying causes of secondary hyperparathyroidism, such as improving calcium and vitamin D intake, has been shown to improve bone density and reduce the risk of fractures in patients with osteoporosis. This further emphasizes the connection between these two conditions and the importance of addressing secondary hyperparathyroidism in the context of bone health.
Managing Secondary Hyperparathyroidism to Prevent Osteoporosis
Since secondary hyperparathyroidism can contribute to the development of osteoporosis, it is crucial to manage this condition in order to protect and maintain bone health. The first step in managing secondary hyperparathyroidism is to identify and treat any underlying causes, such as chronic kidney disease or vitamin D deficiency.
In addition to addressing these causes, maintaining a healthy lifestyle that includes regular exercise, a balanced diet rich in calcium and vitamin D, and avoiding smoking and excessive alcohol consumption can help keep bones strong and reduce the risk of osteoporosis. In some cases, medications may be prescribed to help lower PTH levels and support bone health.
Monitoring Bone Health in Patients with Secondary Hyperparathyroidism
For patients with secondary hyperparathyroidism, it is important to regularly monitor bone health in order to detect any signs of osteoporosis and take appropriate action. This may include regular bone density scans, blood tests to measure calcium and PTH levels, and assessment of fracture risk.
By keeping a close eye on bone health and addressing any issues early on, patients with secondary hyperparathyroidism can lower their risk of developing osteoporosis and maintain strong, healthy bones.
Understanding the Role of Calcium and Vitamin D
Calcium and vitamin D play a crucial role in bone health and in the management of secondary hyperparathyroidism. Calcium is a key component of bone structure and is necessary for proper bone remodeling, while vitamin D is essential for the absorption of calcium from the gut.
Ensuring adequate intake of calcium and vitamin D is important for everyone, but it is particularly crucial for patients with secondary hyperparathyroidism. Addressing deficiencies in these nutrients can help to lower PTH levels, support bone health, and reduce the risk of osteoporosis.
Conclusion: A Strong Connection with Significant Implications
The connection between secondary hyperparathyroidism and osteoporosis is clear and significant. Chronic elevation of PTH levels due to secondary hyperparathyroidism can lead to increased bone resorption, decreased bone formation, and ultimately, a higher risk of osteoporosis and fractures.
Understanding this connection is important for patients and healthcare providers alike, as it highlights the need to address secondary hyperparathyroidism and its underlying causes in order to maintain optimal bone health. With appropriate management and monitoring, it is possible to reduce the risk of osteoporosis and maintain strong, healthy bones throughout life.

Lori Brown
May 7, 2023
Great overview of how secondary hyperparathyroidism drives bone loss!
I love that you broke down the hormone mechanics in simple terms.
Knowing that PTH spikes pull calcium from our skeleton helps explain the fragility.
The link to chronic kidney disease is especially important for patients on dialysis.
Vitamin D deficiency is a silent culprit that many overlook.
Your tip about checking calcium and PTH labs regularly is spot‑on.
Lifestyle tweaks like weight‑bearing exercise can blunt the resorption cascade.
It’s encouraging that correcting vitamin D levels can actually lower PTH.
The article’s reminder to monitor bone density scans every 1‑2 years is practical.
I also appreciate the mention of pharmacologic options such as calcimimetics.
Those agents can reduce PTH secretion without causing hypercalcemia.
For anyone worried about fractures, taking a calcium‑rich diet plus vitamin D3 is a low‑cost safeguard.
I’ve seen patients improve their T‑scores after just three months of supplementation.
Keep spreading this knowledge – empowering patients leads to better outcomes.
Thanks for the thorough piece! :)
Jacqui Bryant
May 13, 2023
Reading this made me realize how important calcium is.
I try to add more dairy and leafy greens to my meals.
A short walk each day also helps my bones stay strong.
Keeping up with doctor appointments is something I now prioritize.
Hope everyone stays healthy!
Paul Luxford
May 20, 2023
The hormonal angle really clarifies why bones get weaker over time.
Seeing the connection to kidney function makes me think about regular check‑ups.
It’s good to know that vitamin D plays a double role in calcium absorption and PTH regulation.
I plan to discuss bone density testing with my doctor soon.
Understanding these mechanisms helps me feel more in control of my health.
Thanks for laying it out in an easy‑to‑follow way.
Nic Floyd
May 27, 2023
From a pathophysiological standpoint secondary hyperparathyroidism induces a catabolic bone remodeling milieu ↑PTH → osteoclast activation ↑bone resorption 🤓💀 the resultant decrease in bone mineral density is quantifiable via DEXA scans 📊 addressing hypocalcemia and vitamin D insufficiency mitigates this cascade 🦴✨ pharmacologic interventions such as calcimimetics further attenuate PTH secretion 🔬💊 overall management necessitates a multidisciplinary approach
Johnae Council
June 3, 2023
Honestly this stuff sounds like a circus of hormones.
Manoj Kumar
June 10, 2023
Isn’t it fascinating how our bodies love to overcompensate for a tiny deficit? You get a cascade of hormone spikes that end up gnawing away at the very scaffolding that holds us together. It’s almost poetic, if you enjoy tragic poetry. The irony of trying to fix low calcium by stealing it from bones is a lesson in unintended consequences. One could argue that evolution forgot to write a user manual for modern medicine. Still, the data is clear – prolonged PTH elevation equals weaker skeletons. So perhaps the smartest move is preventative nutrition rather than reactive drug regimes. Either way, the connection is undeniable, whether we like it or not.
Hershel Lilly
June 17, 2023
I’ve always wondered why the parathyroid glands react so aggressively. It seems the feedback loop is too sensitive in certain chronic conditions. Managing phosphate levels alongside calcium could be a key piece of the puzzle. I’ll bring this up at my next nephrology appointment. Hopefully we can fine‑tune the balance before bone loss becomes severe.
Carla Smalls
June 24, 2023
What a solid summary! It’s empowering to see how lifestyle tweaks can make a real difference. Including calcium‑rich foods, getting safe sun exposure for vitamin D, and staying active are all within our control. Remember to set realistic goals – even small changes add up over time. Keep sharing these insights, they’re invaluable for anyone navigating bone health.
Monika Pardon
July 1, 2023
While the mainstream narrative paints secondary hyperparathyroidism as a mere endocrine hiccup, one must consider the broader context. There are subtle industry pressures to promote pharmaceutical “solutions” over simple nutritional interventions. The literature often highlights calcimimetics while downplaying the efficacy of naturo‑therapeutics. Moreover, certain labs profit from frequent testing, incentivizing a cycle of over‑diagnosis. It would be remiss not to question why calcium supplementation is sometimes dismissed as “ineffective” in some studies. A deeper dive reveals selective data presentation. Let us remain vigilant and seek out independent research. In the end, a balanced approach-addressing dietary intake, sun exposure, and judicious use of meds-is prudent. Transparency is key to truly tackling the bone loss epidemic. Stay informed, stay critical.
Rhea Lesandra
July 8, 2023
Thank you for breaking down such a complex topic into digestible pieces. Your emphasis on both medical and lifestyle strategies resonates with many of us. While the scientific details are crucial, the practical takeaways-like adequate calcium, vitamin D, and regular exercise-are what people can act on immediately. It’s also helpful to remind readers about routine bone density screenings; early detection can change outcomes dramatically. Keep fostering this blend of evidence‑based guidance and actionable advice. We all benefit from shared knowledge and supportive dialogue. Looking forward to more insightful posts like this.
Kasey Marshall
July 15, 2023
Nice breakdown of the mechanisms and treatment options
Dave Sykes
July 22, 2023
Let’s cut to the chase – if you have secondary hyperparathyroidism, you need a multi‑pronged plan now. Start with correcting calcium and vitamin D deficiencies, then evaluate kidney function, and finally consider appropriate meds. Waiting around for bone loss to become severe is not an option. Take charge, schedule those labs, and talk to your specialist about a tailored regimen. Your bones will thank you.
Erin Leach
July 29, 2023
I hear you, Dave, and I appreciate the direct approach. It can be overwhelming, but breaking it down into clear steps makes it manageable. I’ll definitely follow this roadmap and keep my doctor in the loop.
Erik Redli
August 5, 2023
This article oversimplifies the relationship and ignores the genetic factors that play a huge role.
Jennyfer Collin
August 12, 2023
Whilst I respect differing opinions, it is essential to acknowledge that the interplay of genetics and hormonal regulation is well‑documented in peer‑reviewed studies 📚🔍 dismissing the established link without robust evidence undermines scientific discourse. Let us remain grounded in data rather than conjecture.