Potassium Intake Calculator for ACE Inhibitor Users
This calculator helps you understand your potassium intake based on your diet and kidney function. Enter your food choices and kidney function to see if you're staying within safe limits while taking ACE inhibitors.
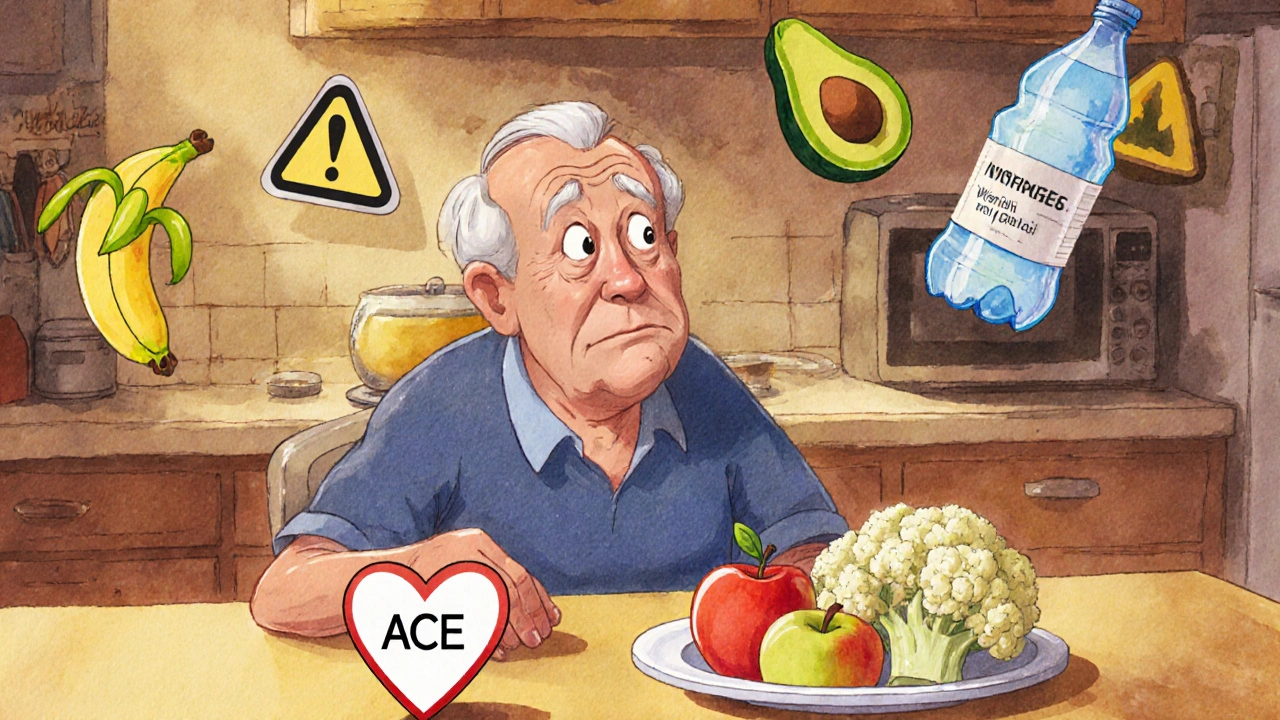
When you're taking an ACE inhibitor for high blood pressure or heart failure, you're doing something good for your heart. But there's a quiet risk hiding in your kitchen: too much potassium. It's not something you hear about often, but it can be dangerous-especially if you have kidney problems. This isn't about avoiding healthy foods altogether. It's about knowing which ones to watch, how much is too much, and what to do if your potassium levels start to creep up.
Why ACE Inhibitors Raise Potassium Levels
ACE inhibitors like lisinopril, enalapril, and ramipril work by blocking a hormone system called RAAS. This helps lower blood pressure and protects your kidneys. But there's a side effect built into the mechanism: less aldosterone. Aldosterone is the hormone that tells your kidneys to flush out extra potassium. When it drops, potassium stays in your blood. That’s how a medication meant to save your heart can accidentally push your potassium into dangerous territory.For most people, this isn’t a problem. Your kidneys handle it fine. But if your kidneys are already struggling-because of diabetes, chronic kidney disease, or just aging-your body can’t keep up. Studies show that 1 in 5 people on ACE inhibitors develop higher-than-normal potassium levels. That number jumps to over 1 in 3 if you’re over 75, have diabetes, or your eGFR (a measure of kidney function) is below 60.
Who’s at Highest Risk?
Not everyone needs to stress about potassium. But if you fall into one of these groups, you should be extra careful:- You’re over 75 years old
- You have diabetes, especially with protein in your urine
- You have heart failure, especially if it’s advanced
- Your kidney function is reduced (eGFR under 60)
- You’re also taking other meds that raise potassium-like spironolactone, trimethoprim, or certain NSAIDs
One study found diabetic patients on ACE inhibitors had nearly a 50% higher chance of hyperkalemia than those without diabetes. That’s not a small bump. It’s a red flag.
Which Foods Are High in Potassium?
You don’t have to give up fruits and veggies. But you do need to know which ones pack a punch. Here’s what to watch:- Bananas: 422 mg per medium fruit
- Oranges and orange juice: 237 mg per fruit, more in juice
- Potatoes (baked with skin): 926 mg each
- Spinach (cooked): 839 mg per cup
- Avocados: 708 mg per cup
- Tomatoes and tomato products (sauce, paste): 292 mg per medium tomato
- Sweet potatoes: 542 mg per medium potato
- Coconut water: 1,150 mg per 16 oz bottle
- Beans and lentils: 600-700 mg per cup cooked
- Dried fruit (raisins, prunes): 300-400 mg per 1/4 cup
Many of these are called "superfoods"-and they are, for most people. But if you’re on an ACE inhibitor with reduced kidney function, even one large baked potato or a bottle of coconut water can push your levels too high. One Reddit user reported a potassium spike after drinking 16 oz of coconut water daily while on lisinopril. That’s not a myth. That’s a real case.
How Much Potassium Is Too Much?
The normal range for potassium in your blood is 3.5 to 5.0 mmol/L. Anything above 5.5 is considered high. Above 6.0? That’s a medical emergency.The National Kidney Foundation recommends that people on ACE inhibitors with eGFR under 45 limit potassium to under 2,000 mg per day. That’s not easy when you’re trying to eat healthy. A single banana and a cup of cooked spinach? That’s already over 1,200 mg. Add a baked potato and a glass of orange juice? You’ve hit your daily limit before lunch.
Here’s a simple rule: if your kidneys aren’t working well, treat potassium like a medication you have to dose carefully. Don’t guess. Measure.
What You Can Still Eat
You don’t need to go on a bland diet. There are plenty of low-potassium options:- Apples, berries, grapes, pineapple
- Cabbage, cauliflower, cucumber, green beans
- Rice, pasta, white bread
- Chicken, turkey, fish (in moderate portions)
- Eggs
- Watermelon (in small amounts-about 1 cup)
- White rice instead of brown
- Drain canned fruits and vegetables before eating
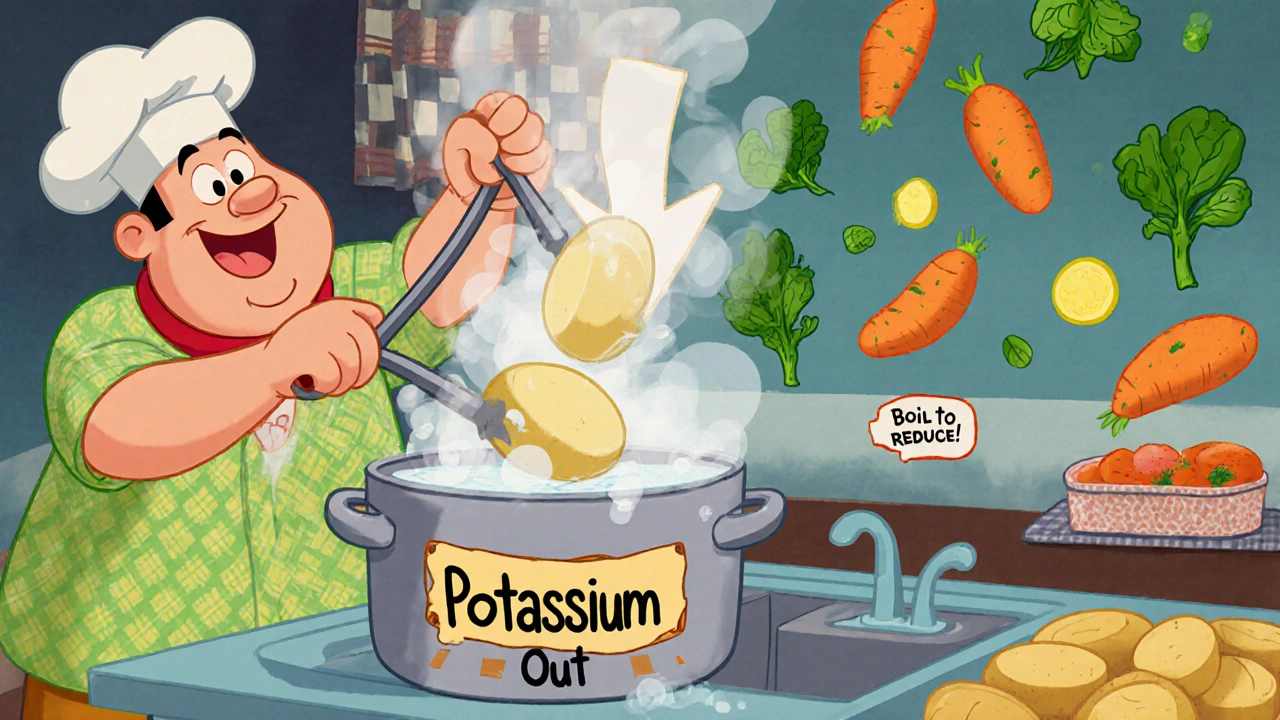
Boiling potatoes, sweet potatoes, or carrots can reduce their potassium by up to 50%. Cut them into small pieces, soak them in water for at least 2 hours, then boil in plenty of fresh water. Drain and rinse again. It’s a small step that makes a big difference.
Monitoring and Testing
Your doctor should check your potassium and kidney function before you start an ACE inhibitor. Then again 7 to 14 days after starting or changing your dose. After that, every 4 months is standard-if you’re stable.If your creatinine rises by up to 30% or your eGFR drops by up to 25%, that’s usually okay as long as you’re not feeling sick and your potassium stays under control. But if your potassium climbs above 5.5, your doctor may adjust your dose, switch your medication, or add a potassium binder.
New Tools to Help You Stay Safe
There’s been real progress in managing this problem. In the past, if your potassium went too high, you had to stop your ACE inhibitor-even if it was helping your heart. Now, there are medications called potassium binders: patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma). These drugs trap potassium in your gut so it leaves your body in your stool instead of building up in your blood.Studies show these binders cut the rate of patients having to stop their ACE inhibitors by over 40%. That’s huge. It means you can keep the heart protection you need without risking your safety.

Practical Tips to Avoid Trouble
Here’s what works in real life:- Ask your doctor for a potassium blood test before starting and 2 weeks after any dose change.
- Get a printed food list from your clinic showing low- and high-potassium choices. Keep it on your fridge.
- Use a free app like "Renal Diet Helper" to track potassium in your meals. Many patients don’t realize how fast it adds up.
- Don’t drink coconut water, sports drinks, or salt substitutes (which often contain potassium chloride).
- Boil high-potassium veggies to reduce their content.
- Never take over-the-counter potassium supplements unless your doctor tells you to.
- If you feel weak, dizzy, or your heart skips beats, get your potassium checked right away.
One study found that patients who got in-person counseling from a renal dietitian were 42% more likely to stick to their potassium limits than those who just got a handout. Talking to someone who knows your situation makes all the difference.
What About Other Medications?
Don’t forget about other drugs. Some common ones can make potassium rise even more:- Trimethoprim (an antibiotic)
- Spironolactone or eplerenone (heart failure meds)
- NSAIDs like ibuprofen or naproxen
- Some herbal supplements (like licorice root)
Combining ACE inhibitors with spironolactone raises the risk of severe hyperkalemia by 58%. That’s why many doctors now avoid this combo unless absolutely necessary.
The Bottom Line
ACE inhibitors are lifesavers. But they come with a responsibility: you need to know how to eat safely with them. You don’t have to give up your favorite foods forever. You just need to be smart about portion sizes, preparation, and timing.Most people who follow these steps never have a problem. The key is early testing, clear guidance, and staying in touch with your care team. If you’re on an ACE inhibitor and have kidney disease or diabetes, talk to your doctor about a referral to a renal dietitian. That single conversation could prevent a hospital visit down the road.
It’s not about fear. It’s about awareness. And awareness saves lives.
Can I still eat bananas if I’m on an ACE inhibitor?
You can, but only in small amounts and only if your kidney function is normal. If your eGFR is below 60 or you have diabetes, one banana a week may be the limit. Always check your potassium levels first. If your levels are already high, avoid bananas and other high-potassium fruits until your doctor says it’s safe.
Is coconut water safe for people on ACE inhibitors?
No, it’s not safe for most people on ACE inhibitors, especially with kidney problems. One 16-ounce bottle contains over 1,150 mg of potassium-nearly half the daily limit for high-risk patients. Many people think it’s a "healthy" drink, but it can trigger dangerous spikes in potassium. Stick to water or low-potassium beverages instead.
Do I need to stop taking my ACE inhibitor if my potassium is high?
Not always. If your potassium is mildly high (5.5-6.0), your doctor may adjust your diet, stop other meds, or prescribe a potassium binder like Lokelma or Veltassa. These drugs let you stay on your ACE inhibitor safely. Only if potassium is very high (above 6.0) or you have symptoms like irregular heartbeat will your doctor consider pausing the medication temporarily.
Can boiling vegetables really reduce potassium?
Yes, it can reduce potassium by up to 50%. Cut the vegetable into small pieces, soak in warm water for at least 2 hours, then boil in plenty of fresh water. Drain and rinse again. This works well for potatoes, sweet potatoes, carrots, and beets. Don’t use the soaking water-pour it away.
How often should I get my potassium checked?
Before starting the ACE inhibitor, then again 7 to 14 days after starting or changing the dose. After that, every 4 months if you’re stable. If you have diabetes, kidney disease, or are over 75, your doctor may want checks every 2-3 months. Don’t skip these tests-they’re simple and can prevent serious problems.
Are there any new treatments for high potassium caused by ACE inhibitors?
Yes. Two new medications-patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma)-bind potassium in your gut and help your body get rid of it through stool. These allow patients to stay on their heart-protecting ACE inhibitors without stopping them. Studies show they reduce the need to discontinue ACE inhibitors by over 40%. They’re not for everyone, but they’re a game-changer for high-risk patients.
What should I do if I feel weak or my heart is racing?
These can be signs of high potassium. Stop eating high-potassium foods immediately and contact your doctor or go to an urgent care clinic. A simple blood test can confirm your potassium level. Don’t wait. High potassium can cause dangerous heart rhythms. It’s better to get checked and be safe than to risk a cardiac emergency.

David Cunningham
November 24, 2025
Man, I just found out my grandpa’s on lisinopril and was chugging coconut water like it’s Gatorade. He’s 78, diabetic, eGFR 42… and he thought it was "healthy hydration." I almost had a heart attack reading this. Thanks for the wake-up call.
Holly Schumacher
November 24, 2025
Let me just say this with surgical precision: the author didn’t just write an article-they performed a public service. The formatting is impeccable, the data is sourced, and the tone avoids fearmongering while still conveying urgency. This is how medical education should be done. Also, boiling potatoes? Genius. Why didn’t anyone tell me this before? I’ve been eating baked sweet potatoes like a caveman.
Shawn Daughhetee
November 24, 2025
so i’ve been on enalapril for 3 years and never thought twice about my banana habit… until i got dizzy last week. turned out my k was 5.8. scary stuff. now i stick to apples and boil my veggies. life’s changed but i’m alive so i guess that’s win
Danny Nicholls
November 24, 2025
Boiling potatoes = 50% less potassium?? 🤯 I’m gonna try this tomorrow with my loaded baked potatoes 🥔🔥 thanks for the tip!! also anyone else use Renal Diet Helper? it’s wild how fast potassium adds up 😅
New Yorkers
November 25, 2025
Oh so now we’re policing what elderly people eat because Big Pharma wants to keep their drugs on the market? Let me guess-the next thing you’ll say is that sunlight causes skin cancer so don’t go outside. This is medical paternalism dressed up as education. People have been eating bananas for centuries. Your kidneys aren’t broken just because you’re on a pill.
Justin Daniel
November 25, 2025
I get where you're coming from, New Yorkers. But this isn't about control-it's about risk. If your kidneys are already struggling, adding 1,150 mg of potassium in one bottle of coconut water is like pouring gasoline on a smoldering fire. I've seen patients in the ER because they thought "natural" meant "safe." It doesn't. The data here isn't opinion-it's clinical reality. And for the record, I'm not on any meds. I just work in nephrology.
Michael Fitzpatrick
November 26, 2025
Look, I’ve been on ACE inhibitors for 8 years with CKD stage 3, and I still eat spinach, sweet potatoes, and the occasional banana. But here’s the thing-I track everything. I use the app, I boil my veggies, I get tested every 3 months, and I avoid salt substitutes like the plague. It’s not about deprivation-it’s about awareness. This post didn’t scare me. It empowered me. And honestly, if you’re not monitoring your potassium, you’re playing Russian roulette with your heart. Not because you’re dumb, but because nobody told you. Now you know.
Latonya Elarms-Radford
November 27, 2025
There’s a profound existential tension here, isn’t there? We are told to eat the rainbow-yet the rainbow contains potassium bombs disguised as superfoods. We are told to honor the body, yet the body betrays us through aging kidneys. We are told to trust science, yet science gives us drugs that save our hearts but slowly poison our blood. Is this not the tragedy of modern medicine? To be saved by a pill only to be haunted by its shadow? I don’t eat bananas anymore. I eat silence. And I weep for the avocado I once loved.
Melvina Zelee
November 27, 2025
omg i just realized i’ve been eating 2 cups of spinach every day with my smoothie and i’m on ramipril… my kidneys are fine but still… maybe i should boil it? and also i’ve been drinking coconut water after yoga-wait nope no more. thank you for this. i’m saving this post. also i spelled potassium wrong in my notes like 17 times 😅
Robin Johnson
November 28, 2025
Stop panicking. Start planning. If you’re on an ACE inhibitor and have diabetes or kidney issues, your potassium level isn’t a mystery-it’s a number you can control. Get the test. Get the list. Get the app. Boil the damn potato. Don’t drink coconut water. Simple. Not sexy. But it works. You don’t need a dietitian to tell you this-you just need to care enough to act. And if you don’t? Then you’re not ready for this conversation. And that’s okay. But don’t blame the medicine. Blame the silence.
Mark Williams
November 28, 2025
Per the KDIGO 2022 guidelines, ACEi-induced hyperkalemia is classified as a Class IIa indication for potassium binders in patients with eGFR < 45 and persistent K+ > 5.0 mmol/L. The number needed to treat (NNT) to prevent one discontinuation of RAASi is approximately 4.3. Veltassa has demonstrated a 60% reduction in hyperkalemia recurrence over 12 months versus placebo in the PEARL-HF trial. This isn’t just anecdotal-it’s evidence-based pharmacotherapy with real-world clinical impact.
Ravi Kumar Gupta
November 29, 2025
In India, we have a saying: "A medicine is a gift only if you know its price." My uncle took lisinopril and ate 3 bananas a day because "he felt fine." He ended up in the ICU with cardiac arrhythmia. We didn’t know about potassium. No one told us. This article? It’s the kind of knowledge that saves lives in places where doctors are scarce. Thank you for writing this. I’m sharing it with my family in Delhi.
Rahul Kanakarajan
November 29, 2025
Wow. So now I’m supposed to give up my avocado toast and sweet potato fries because I’m 65 and on a blood pressure pill? What’s next? Are we gonna ban oxygen because some people have COPD? This is ridiculous. People are dying from depression because they think they can’t eat healthy anymore. This article is fear-mongering dressed up as science. I’m not changing my diet because some algorithm told me to.
Nikhil Chaurasia
November 30, 2025
Respectfully, I’ve seen too many patients in my clinic who were told to "just avoid potassium" and then starved themselves of fruits and greens until they got weak and malnourished. The goal isn’t to eliminate-it’s to balance. Boiling, portion control, timing meals, and regular labs-that’s the real path. This post nails it. I’ve printed it and put it on my wall. Thank you for not being alarmist but still being clear.
Melvina Zelee
December 1, 2025
also just a heads up-i asked my doctor about lokelma and he said it’s like $600 a month and insurance barely covers it. so for most people, boiling potatoes and skipping coconut water is still the only option. just saying. not everyone can afford the fancy pills. but hey, at least we know how to save ourselves the old-fashioned way 💪