Acetaminophen is in almost every medicine cabinet - but most people don’t know how dangerous it can be
You take it for a headache. Your kid takes it for a fever. You grab a cold medicine because you’re feeling under the weather. All of these are normal. But here’s the thing: acetaminophen is hiding in more than 600 different products - from pain relievers to sleep aids to cough syrups. And if you don’t know what you’re taking, you could be poisoning your liver without even realizing it.
Every year in the U.S., more than 56,000 people end up in the emergency room because of acetaminophen. Over 26,000 are hospitalized. About 500 die. And here’s the worst part: most of these cases aren’t intentional. People aren’t trying to hurt themselves. They’re just confused.
Acetaminophen - the active ingredient in Tylenol - is safe when you follow the label. But the line between safe and dangerous is thin. Take just two extra pills over 24 hours, and you could be in serious trouble. Especially if you’re drinking alcohol. Or taking another medicine that also has acetaminophen. Or if you have a history of liver problems.
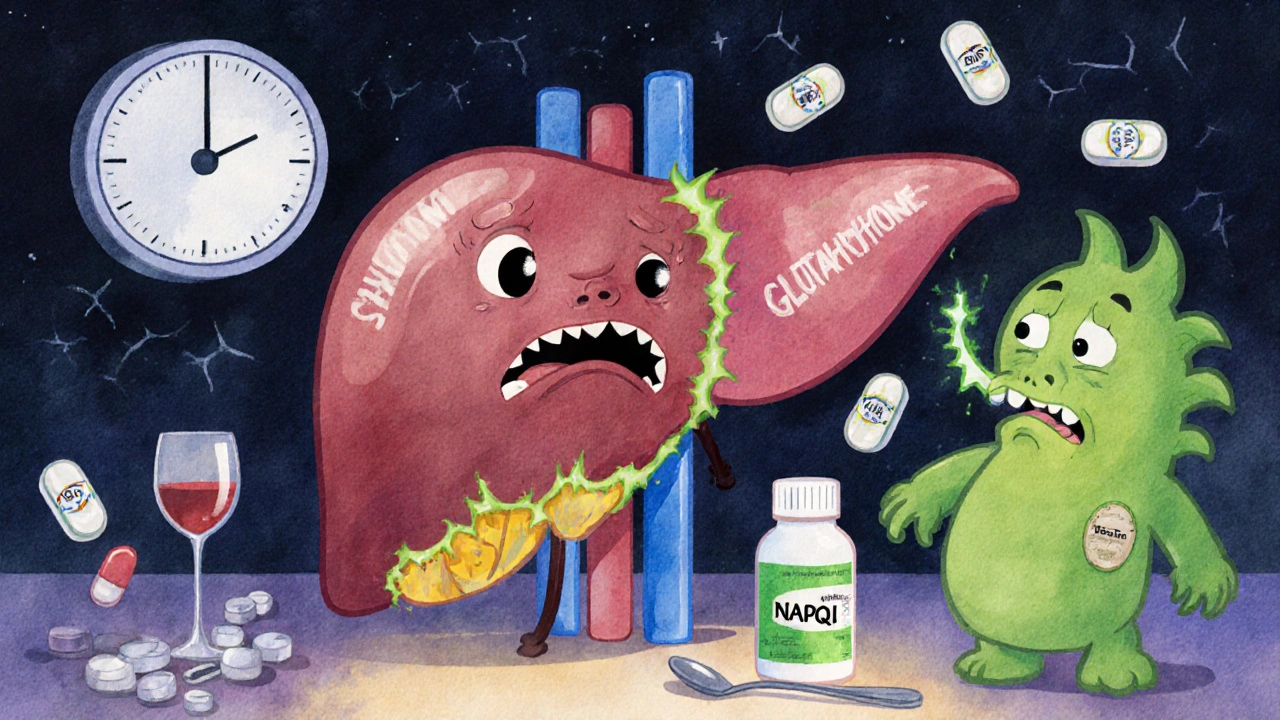
How acetaminophen damages the liver - and why it happens silently
Your liver breaks down acetaminophen every time you take it. At normal doses, it handles the job fine. But when you take too much - even just a little too much - your liver gets overwhelmed. It starts producing a toxic byproduct called NAPQI. Normally, your body neutralizes it with glutathione. But when you overload the system, glutathione runs out. And then NAPQI starts eating away at liver cells.
This isn’t like a stomach ache that comes right away. Acetaminophen toxicity sneaks up on you. In the first 24 hours, you might feel nothing. Or just a little nausea. That’s Stage I. By the time your liver is really hurting - Stage II and III - it’s often too late to reverse the damage without urgent treatment.
By day three, symptoms get serious: severe pain under your right ribs, yellowing skin (jaundice), confusion, vomiting, dark urine. Your liver enzymes skyrocket. Some patients see levels over 10,000 IU/L - normal is under 40. At this point, you’re at risk of liver failure, kidney damage, and even death.
The biggest danger? You’re not taking just one medicine
Most overdoses aren’t from taking 10 Tylenol pills at once. They’re from taking Tylenol and a cold medicine and a prescription painkiller - all without realizing they all contain acetaminophen.
Here’s how it happens:
- You take two extra-strength Tylenol (1,000 mg) for your back pain.
- Later, you take a cold tablet labeled “DayQuil” - which also has 325 mg of acetaminophen.
- At night, you take NyQuil - another 650 mg.
- That’s 2,000 mg in 12 hours. You’re already halfway to the danger zone.
And that’s just three products. Some people take four or five. The CDC says 12% of pediatric overdoses happen because parents use kitchen spoons to measure liquid medicine. A tablespoon isn’t a teaspoon. And adult formulations? Never give them to kids. Ever.
Even more dangerous are prescription combos like Vicodin or Percocet. They contain acetaminophen too - up to 325 mg per pill. If you’re already taking Tylenol on the side, you’re doubling up without knowing it.
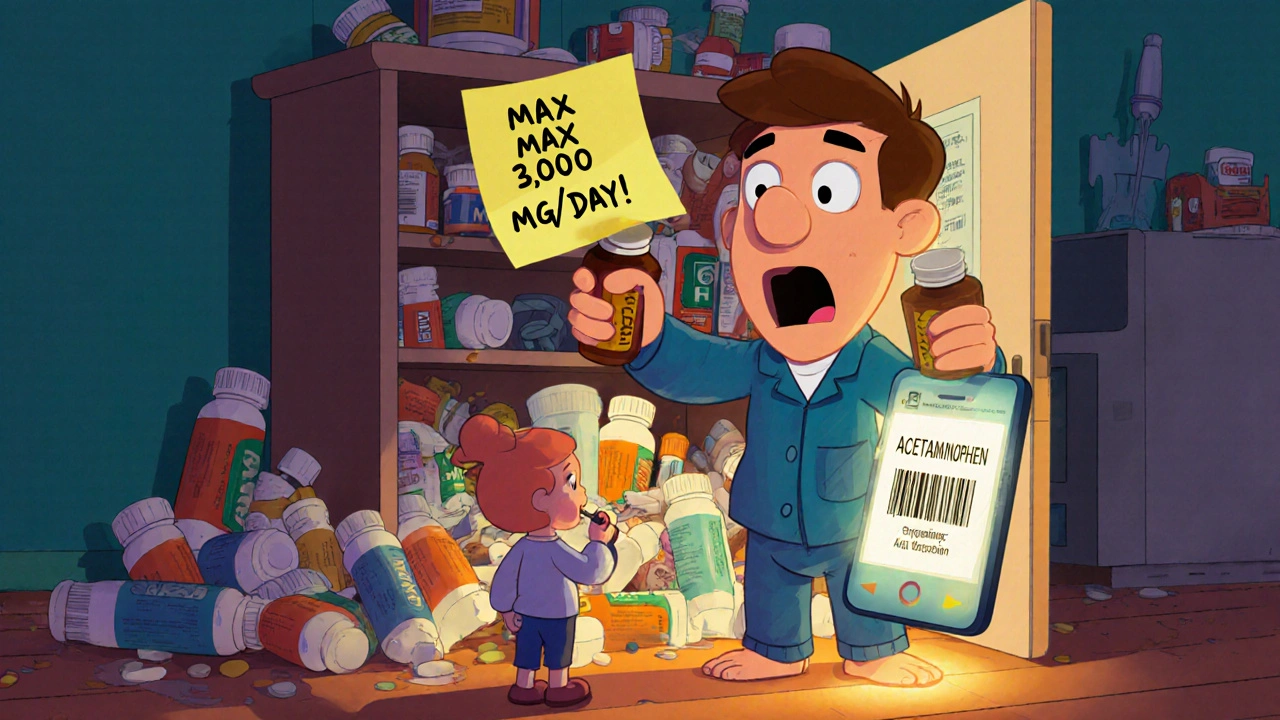
What’s the real safe dose? It’s not what you think
The old rule - 4,000 mg per day - is outdated for many people. The FDA now recommends a maximum of 3,000 mg per day for most adults, especially if you’re over 65, have liver disease, or drink alcohol regularly.
Here’s what you need to know:
- Regular Tylenol: 325 mg per tablet - max 8 tablets per day (2,600 mg)
- Extra Strength Tylenol: 500 mg per tablet - max 6 tablets per day (3,000 mg)
- Children: 10-15 mg per kg of body weight, every 4-6 hours - no more than 5 doses in 24 hours
- Never exceed 7.5 grams in one day - that’s the point where liver damage becomes likely
And if you drink alcohol - even just 2-3 drinks a day - your liver’s ability to process acetaminophen drops by up to 50%. That means your safe dose could be as low as 2,000 mg per day.
How to prevent an overdose - simple steps that save lives
Preventing acetaminophen overdose isn’t complicated. It’s about habits.
- Read every label. Look for “acetaminophen” or “APAP.” It’s often printed in small print. If you see it, stop taking any other product with it.
- Use a medication tracker. Write down what you take and when. Use a notebook or a free app. Don’t rely on memory.
- Never mix with alcohol. Even one drink a day increases your risk. If you drink, cut acetaminophen out completely or use less than 2,000 mg per day.
- Use the right measuring tool. For kids, always use the dosing cup or syringe that comes with the bottle. Never use a kitchen spoon.
- Ask your pharmacist. If you’re on multiple meds, ask: “Does this contain acetaminophen?” They’ll tell you - and they’re trained to catch hidden combinations.
Also, check your cabinet. If you have three different cold medicines, you probably have three different sources of acetaminophen. Toss the extras. Keep only one.
What to do if you think you’ve taken too much
If you suspect an overdose - even if you feel fine - act fast.
- Call Poison Control immediately: 1-800-222-1222 (U.S. and Canada). They’re available 24/7.
- Go to the ER. Don’t wait for symptoms. By the time you feel sick, your liver may already be damaged.
- Bring all your meds with you - including the bottles.
There’s an antidote: N-acetylcysteine (NAC). If given within 8 hours of overdose, it’s 90% effective at preventing liver damage. After 16 hours? That drops to 60%. Time is everything.
One man in Edmonton took 8 extra-strength Tylenol over 10 hours for a bad migraine. He felt fine until the next morning - then he started vomiting and his skin turned yellow. He called Poison Control. They told him to go to the ER. He got NAC within 6 hours. His liver enzymes returned to normal in 10 days. He says: “I didn’t know I was in danger. Now I check every label.”
Why labeling isn’t enough - and what’s changing
The FDA requires all acetaminophen products to have a “Liver Warning.” But a 2022 study found only 38% of people could even identify acetaminophen on the label. Most saw “Tylenol” and didn’t realize it was the same thing as “APAP” or “acetaminophen.”
New rules are coming. The FDA is pushing for bigger, bolder text on labels. Some companies are testing barcode scanners on phones that can scan your meds and warn you if you’re over the limit. These tools could be game-changers.
But until then, the responsibility is on you. Don’t assume. Don’t guess. Don’t rely on brand names. Know what’s in your medicine.
Acetaminophen isn’t evil - but it’s not harmless either
It’s still the safest painkiller for people with stomach ulcers, kidney disease, or heart problems. It doesn’t cause bleeding like ibuprofen. It’s the go-to for pregnant women and kids. But safety only exists when you respect the limits.
Think of it like driving: a car is safe when you follow the speed limit. Go too fast, and you crash. Acetaminophen is the same. Take it as directed - and you’re protected. Go over the line - even just a little - and your liver pays the price.
Can I take acetaminophen if I drink alcohol?
If you drink alcohol regularly - even just 2-3 drinks a day - your risk of liver damage from acetaminophen increases significantly. Experts recommend limiting acetaminophen to no more than 2,000 mg per day if you drink, or avoiding it entirely. Never take acetaminophen after binge drinking. Your liver is already under stress.
Is it safe to take acetaminophen every day?
Long-term daily use - even at low doses - can lead to liver damage over time, especially if you have underlying liver disease, are overweight, or take other medications. If you need pain relief daily, talk to your doctor. There may be safer alternatives. Don’t use acetaminophen as a daily habit without medical advice.
What’s the difference between Tylenol and generic acetaminophen?
There’s no difference in the active ingredient. Generic acetaminophen contains the exact same chemical as Tylenol. The only differences are price and inactive ingredients like fillers or coatings. Generic versions are just as effective - and just as dangerous if misused. Always check the label, no matter the brand.
Can children take adult acetaminophen?
Never. Adult formulations contain much higher doses. A single adult tablet can be toxic to a child. Always use products labeled for children and dose strictly by weight. Use the measuring device that comes with the bottle - not a kitchen spoon.
What are the signs of acetaminophen poisoning?
Early signs (0-24 hours): nausea, vomiting, loss of appetite, sweating, pale skin. Later signs (24-72 hours): pain under the right ribs, dark urine, yellow eyes or skin, confusion. If you’ve taken too much and feel sick - even hours later - seek help immediately. Symptoms can be delayed.
Is there a blood test to check for acetaminophen overdose?
Yes. Hospitals test blood levels of acetaminophen and liver enzymes (ALT, AST). If the acetaminophen level is above the treatment line on the Rumack-Matthew nomogram - which doctors use to predict liver damage - they’ll give NAC right away. Don’t wait for symptoms. Get tested if you suspect an overdose.
Next steps: Make your medicine cabinet safer today
Here’s what to do right now:
- Go to your medicine cabinet. Pull out every bottle with “acetaminophen” or “APAP” on the label.
- Write down how much each contains per dose.
- Add up your total daily intake if you take them all.
- Throw out any duplicates - you only need one pain reliever.
- Put a sticky note on your main bottle: “Max 3,000 mg/day. No alcohol.”
Acetaminophen saves lives when used right. But it can end them when used carelessly. Know what’s in your meds. Respect the dose. When in doubt - call Poison Control. It’s free. It’s fast. And it might save your liver.


Brian Bell
November 14, 2025
This is wild. I had no idea so many cold meds had acetaminophen. I’ve been taking DayQuil and Tylenol together for years 😅. Time to clean out my cabinet.
Ryan Anderson
November 15, 2025
I’ve been using a medication tracker app since my dad had a near-overdose. It’s a game-changer. Also, I put a sticky note on my Tylenol bottle: "NO ALCOHOL. MAX 3K MG." Simple, but it works. 🛡️
Sean Hwang
November 16, 2025
i used to think tylenol was totally safe til i read this. now i always check labels. even the ones that say "pain relief". apap = bad news if you dont know. thanks for the heads up!
Ashley Durance
November 17, 2025
The fact that people still use kitchen spoons to measure children’s medicine is horrifying. This isn’t a parenting fail-it’s a public health catastrophe waiting to happen. You wouldn’t measure fuel for your car with a soup spoon. Why is this acceptable?
Hrudananda Rath
November 18, 2025
The casual disregard for pharmacological precision among the general populace is nothing short of a societal pathology. One does not casually ingest hepatotoxic agents with the same nonchalance one might consume aspirin at a picnic. The FDA’s recommendations are not suggestions-they are the bare minimum of rational self-preservation. And yet, we persist in our collective ignorance, as though the liver were an inexhaustible reservoir of biological goodwill.
Jane Johnson
November 19, 2025
I’m surprised this isn’t a bigger scandal. The pharmaceutical industry profits from confusion. They hide acetaminophen in plain sight. It’s not negligence-it’s designed.
kshitij pandey
November 19, 2025
In India, we call it paracetamol and it's everywhere. But most people don’t know it’s the same as Tylenol. I’ve started telling my family: "Check the small letters, not the big brand." One less trip to the hospital, one more day healthy. 🙏
Peter Aultman
November 20, 2025
this post saved my life honestly. i was taking nyquil and tylenol every night for migraines. felt fine till i started getting dizzy. called poison control and they said i was at 2800mg in 12 hours. i stopped cold turkey and now i use ibuprofen instead. thanks for the wake up call
Nathan Hsu
November 21, 2025
I must emphasize, with great urgency and a sense of moral gravity: acetaminophen is not a benign substance! It is, in fact, a biochemical time bomb-silent, insidious, and lethally efficient-when misused! Please, for the love of all that is hepatic, read the label! Read it again! And again! And if you’re still unsure? Consult a pharmacist! Do not gamble with your liver!
Barry Sanders
November 21, 2025
Americans think they can medicate their way out of everything. You take Tylenol for a headache, then a cold pill, then a sleep aid. You don’t need all that junk. Just go to bed. Stop taking pills like candy.
Brittany C
November 22, 2025
The pharmacokinetic burden of polypharmacy in the context of acetaminophen co-ingestion is a well-documented risk factor for hepatotoxicity, particularly in individuals with suboptimal glutathione reserves. The NAC window is critical, yet underutilized due to delayed presentation.
Sean Evans
November 23, 2025
People are dumb. Not just careless-dumb. You think your liver is a sponge? It’s an organ. It doesn’t get a second chance. If you’re still taking Tylenol with a beer, you’re not a patient-you’re a liability.
Anjan Patel
November 25, 2025
I used to think acetaminophen was harmless. Then I saw my cousin in the ICU after taking "just a few extra pills" for his back pain. He’s lucky he didn’t die. Now I tell everyone: if you don’t know what’s in it, don’t take it. Period.
Scarlett Walker
November 25, 2025
I just checked my cabinet and found 4 different bottles with APAP. I threw out 3. I feel so much better already. This post was a gift. Thank you.
Eleanora Keene
November 27, 2025
You're doing amazing work by sharing this. So many people don't know the risks. I'm going to print this out and leave it on the fridge. My kids are teens now-they need to know this before they start taking meds on their own. 💪
Chris Ashley
November 28, 2025
i took 2 tylenol and a cold pill last night and now i’m paranoid. should i go to the er? i feel fine but idk what to do
Scott Saleska
November 28, 2025
I’ve been a pharmacist for 18 years. The most common question I get isn’t about side effects-it’s "Is this okay to take with Tylenol?" People have no idea what’s in their meds. This post should be mandatory reading before you buy any OTC drug.
Joe Goodrow
November 30, 2025
This is why we need to stop letting foreign-made drugs flood our market. In America, we know what’s in our medicine. You don’t see this kind of mess in Europe or Canada. We need better labeling laws-and enforcement.
Don Ablett
December 1, 2025
The Rumack-Matthew nomogram remains the gold standard for clinical decision-making in acetaminophen overdose. The 8-hour window for NAC administration is not arbitrary-it is empirically derived from hepatic glutathione depletion kinetics. Delayed presentation correlates directly with mortality. Time is liver.