What Is Allergic Asthma?
Allergic asthma is the most common form of asthma, affecting about 60% of the 25 million Americans with the condition. It’s not just regular asthma-it’s asthma that flares up when your immune system overreacts to harmless substances like pollen, dust mites, or pet dander. These substances, called allergens, trigger your body to release IgE antibodies, which then set off a chain reaction: mast cells burst open, eosinophils flood your airways, and your bronchial tubes tighten. The result? Wheezing, coughing, chest tightness, and shortness of breath-often worse at night or during allergy season.
This isn’t just a guess. Doctors confirm it with tests. A skin prick test showing a wheal larger than 3mm, blood tests with IgE levels above 100 kU/L, or sputum with more than 3% eosinophils all point to allergic asthma. Unlike non-allergic asthma, which often starts in adulthood and has no clear trigger, allergic asthma usually begins in childhood. Studies show the average age of onset is just 12.3 years old.
Top Triggers You Can’t Ignore
If you have allergic asthma, knowing your triggers isn’t optional-it’s life-changing. The biggest culprits fall into two categories: outdoor and indoor.
Outdoor triggers follow the seasons. Tree pollen hits hardest from February to April, especially in March, with counts hitting 10-20 grains per cubic meter. Grass pollen spikes in June, sometimes exceeding 100 grains per cubic meter. Then comes ragweed in September-this one’s the worst. When ragweed pollen hits over 100 grains per cubic meter, emergency room visits for asthma jump dramatically.
Indoor triggers are always there, even in winter. Dust mites live in bedding, carpets, and upholstered furniture. They thrive when humidity is above 50%. In fact, 84% of U.S. homes have enough dust mite allergen (over 2 µg/g of dust) to trigger reactions. Cat allergen (Fel d 1) is even sneakier-it sticks to clothes, carpets, and walls. It’s found in 79% of U.S. homes, even if no cat lives there. Dog allergen (Can f 1) shows up in 67% of homes. Mold, especially Alternaria, explodes after thunderstorms. When spore counts go above 500 per cubic meter, ER visits for asthma rise 3.5 times.
How to Avoid Allergens (Real Strategies That Work)
Avoiding allergens sounds simple. But most people don’t do it right. Here’s what actually works, backed by data from the EPA, CDC, and peer-reviewed studies.
- Bedding overhaul: Use allergen-proof covers on your mattress, box spring, and pillows. Brands like AllerZip Pro are tested to block dust mites. One user saw their peak flow jump from 380 to 470 L/min after switching.
- Wash bedding weekly in hot water: Water at 130°F or higher kills 90% of dust mites. Cold water? Almost no effect.
- Control humidity: Keep indoor humidity between 30-50%. Use a hygrometer to monitor. At 45% RH, dust mite allergen drops from 20 µg/g to just 0.5 µg/g.
- Use a HEPA vacuum twice a week: Regular vacuums blow allergens back into the air. A Dyson V15 or similar HEPA model reduces cat allergen by 42%.
- Keep windows closed during high pollen days: When tree pollen hits 9.7 grains per cubic meter, close windows. Use air conditioning instead.
- Shower after being outside: Pollen sticks to hair and skin. Showering reduces allergen transfer to bedding by 70%.
- Wear an N95 mask during yard work: It cuts pollen exposure by 85%. Don’t just rely on a dust mask-it’s not enough.
- Remove carpets: Hard floors are easier to clean. If you keep carpet, steam clean it monthly.
One study found that people who followed these steps reduced their asthma medication use by up to 40% in just six months.

Immunotherapy: The Only Treatment That Changes the Course of Allergic Asthma
Medications like inhalers and antihistamines help you breathe better today. But immunotherapy is the only treatment that changes your body’s long-term response to allergens.
There are two main types: subcutaneous immunotherapy (SCIT) and sublingual immunotherapy (SLIT).
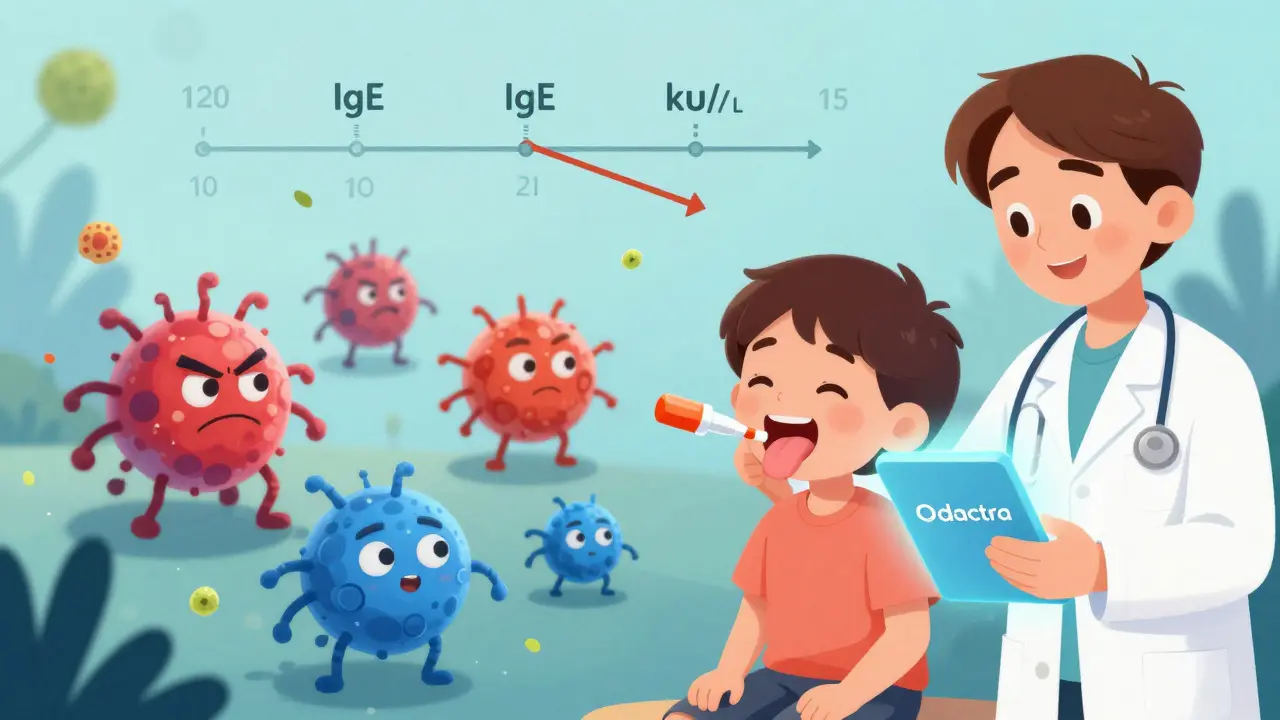
SCIT means allergy shots. You get weekly injections for 4-6 months, slowly building up to a maintenance dose. After that, you go monthly for 3-5 years. Studies show 70-80% of patients see major improvement after 12-18 months. A 12-year-old with severe cat allergy dropped their IgE from 120 kU/L to 15 kU/L after three years of shots-and passed a challenge test with no reaction.
SLIT is daily tablets or drops under the tongue. It’s less invasive. Grastek (for grass) and Odactra (for dust mites) are FDA-approved. It’s convenient, but 78% of users get oral itching in the first month. That’s why some quit. Still, in the MILO trial, SLIT reduced asthma symptoms by 35%-compared to just 15% with inhaled steroids alone.
Immunotherapy doesn’t just reduce symptoms. It cuts medication use by up to 28% over 10 years. And it lowers the risk of developing new allergies. That’s huge.
What Doesn’t Work (And Why People Get Frustrated)
Not all advice is equal. Some popular fixes don’t help-or make things worse.
- Essential oils: No evidence they help asthma. Some (like eucalyptus) can irritate airways.
- Air purifiers without HEPA filters: Ionizers and UV lights don’t remove allergens. Only HEPA does.
- Just taking antihistamines: They help sneezing, but not asthma. You still need inhaled steroids or immunotherapy.
- Waiting until you have symptoms: Prevention beats reaction. Start avoidance before allergy season hits.
And here’s a big one: not testing properly. About 30% of people diagnosed with allergic asthma don’t actually have type 2 inflammation. That means they’re getting expensive biologics (like omalizumab) that cost $30,000-$40,000 a year-and do nothing for them. Blood eosinophils and FeNO tests are critical before starting these drugs.
What’s New in 2026: Precision Asthma Care
The field is moving fast. New tools are making management smarter and more personal.
- AI-powered apps: AsthmaIQ, launched in April 2024, tracks your symptoms, medication, pollen levels, and even indoor air quality. It predicts your next flare-up with 92% accuracy.
- Nasal sensors: The Allergen Insight sensor (FDA breakthrough in 2023) detects allergens as low as 0.1 µg/m³ and alerts your phone.
- Genetic testing: The NIH is testing a gene marker (rs230548) that predicts who will respond to immunotherapy-with 85% accuracy.
- Faster immunotherapy: CAT-PAD, a new peptide therapy for cat allergy, cuts the build-up phase from 6 months to just 8 weeks.
- New biomarkers: High IgE to Alternaria (>17.5 kU/L) means you’re 4.7 times more likely to have a severe asthma attack.
By 2030, experts predict combination therapy-biologics plus immunotherapy-could control 75% of allergic asthma cases, up from just 50% today. That’s a game-changer.
Insurance, Cost, and Access
Immunotherapy is expensive, but coverage is improving. In the U.S., Medicare covers 80% of SCIT costs under Part B. You pay about $18.90 per shot. SLIT tablets are often covered too. Still, only 15% of allergic asthma patients get immunotherapy-up from 8% in 2015. In Europe, where healthcare is universal, that number is 28%.
Why so low? Cost isn’t the only barrier. Many patients don’t know it’s an option. Others fear needles. Others quit because of side effects. But for those who stick with it, the payoff is huge: fewer ER visits, less medication, and better quality of life.
Can allergic asthma go away on its own?
In some children, allergic asthma improves with age-but it rarely disappears completely. The immune system doesn’t forget the allergen. Without proper management, symptoms often return in adulthood. Immunotherapy is the only treatment proven to change long-term outcomes and reduce the chance of relapse.
Is immunotherapy safe for kids?
Yes. Both SCIT and SLIT are approved for children as young as 5. SLIT is often preferred for kids because it’s needle-free. Studies show it’s just as effective as shots and has fewer severe side effects. The most common issue is mild oral itching, which usually fades after a few weeks.
Do I still need my inhaler if I get immunotherapy?
Yes-at least at first. Immunotherapy takes 12-18 months to start working. You’ll still need your rescue inhaler and controller meds during that time. But as your body gets used to the allergens, you’ll likely need less medication. Many patients cut their inhaler use in half after 2-3 years of therapy.
Can I do allergen avoidance and immunotherapy at the same time?
Absolutely. In fact, it’s the best approach. Avoidance reduces your exposure, so your body isn’t constantly fighting allergens. Immunotherapy teaches your immune system to tolerate them. Together, they’re more powerful than either alone. Studies show this combo reduces exacerbations by up to 60%.
What if I can’t afford immunotherapy?
Start with allergen avoidance. It’s free or low-cost and works for most people. Wash bedding weekly, use HEPA filters, control humidity. These steps alone can cut symptoms by 30-40%. If your symptoms persist, talk to your allergist about payment plans or patient assistance programs. Many drug manufacturers offer discounts for SLIT tablets.
What’s Next?
If you have allergic asthma, your next step is simple: get tested. Ask your doctor for a skin prick test or IgE blood test. If you’re allergic, work with an allergist to build a plan-avoidance first, then immunotherapy if needed. Don’t wait for another attack. The tools to take control are here. And they’re more effective than ever.


Melissa Melville
February 2, 2026
So basically if you don't want to die indoors, just live in a plastic bubble and never touch anything? Sounds like a fun life.
Bryan Coleman
February 3, 2026
HEPA vacuums are a game changer. I got a Dyson and my wife's asthma attacks dropped by like 60%. Also shower after being outside? Duh. But so many people forget that.
Naresh L
February 4, 2026
I wonder if the immune system's overreaction is evolution's mistake-or perhaps a misfired defense mechanism from a time when mold spores meant something far deadlier than a sneeze.
Sami Sahil
February 5, 2026
Bro just wash your sheets every week and use AC. No need to spend 30k on shots. I did this and my peak flow went from 340 to 480. Life changed.
franklin hillary
February 6, 2026
Immunotherapy isn't a cure-it's a reset button for your immune system. And yes, it's worth every penny. The real tragedy is people waiting until they're on oxygen before they try it.
Bob Cohen
February 7, 2026
I'm all for avoidance, but the fact that 79% of homes have cat allergen even without cats? That's wild. I think we need a national pet allergen registry. Just saying.
Ishmael brown
February 8, 2026
Air purifiers are a scam. The real solution? Stop living in sealed plastic boxes and let your body adapt. Also, why is no one talking about 5G triggering mast cells?
Aditya Gupta
February 9, 2026
Wash sheets. Keep dry. Use HEPA. Done. No need for fancy apps or sensors. Simple works.
Nancy Nino
February 10, 2026
I must express my profound admiration for the meticulous research presented herein. Truly, a paradigm-shifting exposition on allergen management.
June Richards
February 10, 2026
Ugh. I've been doing all this for years and still end up in the ER. This post is just guilt-tripping people who already suffer. 🙄
Lu Gao
February 11, 2026
You mentioned '84% of U.S. homes have dust mite allergen above 2 µg/g.' That statistic is from a 2019 CDC study. You should cite it properly.
Angel Fitzpatrick
February 13, 2026
Allergens are a bioweapon. The EPA and WHO are hiding the truth. They're seeding pollen with nano-tech to control populations. You think the 'N95 mask cuts exposure by 85%' is coincidence? Think again.
Nicki Aries
February 14, 2026
I was diagnosed at 11. My mom made me wear an N95 while raking leaves. I hated it. But now, at 34, I'm off all inhalers. I didn't just survive-I thrived. If you're reading this and scared? Start small. One habit. One week. You can do this.
Nidhi Rajpara
February 15, 2026
I have a question: If immunotherapy reduces new allergies, why is the rate of allergic diseases still rising? Is this not contradictory?