Every year, the FDA approves hundreds of generic drugs - and each one saves patients and the healthcare system millions, sometimes billions, of dollars. But how much do these approvals actually save? And why do the numbers jump from year to year? The answer isn’t just about how many generics get approved - it’s about which drugs they replace.
What the FDA Tracks: Savings from New Generic Approvals
The FDA doesn’t just count how many generic drugs get approved. It tracks how much money those new approvals save in the first 12 months after they hit the market. This is called first-year savings from new generic approvals. It’s not the total savings from all generics in use - it’s the immediate drop in price when a brand-name drug loses its monopoly.
Here’s what happened in recent years:
- 2018: $2.7 billion saved
- 2019: $7.1 billion saved - the highest on record
- 2020: $1.1 billion saved
- 2021: $1.37 billion saved
- 2022: $5.2 billion saved
Why such wild swings? Because savings depend on which brand-name drugs lose patent protection. In 2019, several high-cost drugs - like the cholesterol medicine Repatha and the diabetes drug Januvia - went generic all at once. That pushed savings to a record high. In 2020, fewer big-ticket drugs expired, so savings dropped sharply. In 2022, major approvals included generics for the blood thinner Pradaxa and the asthma drug Advair, both of which had annual sales over $3 billion. That’s why savings jumped back up.
The FDA found that when a new generic enters the market, the brand-name version’s price typically drops by more than 70% within a year. The generic itself usually sells for 80-95% less than the brand. That’s not a small discount - it’s life-changing for people paying out of pocket.
Total Generic Savings: What the Industry Reports
The FDA’s numbers show the impact of new entries. But the real picture of savings comes from the Association for Accessible Medicines (AAM). They measure total savings from all generic drugs in use during a calendar year - not just the new ones.
In 2023, generics and biosimilars saved the U.S. healthcare system $445 billion. That’s more than the entire annual budget of the Department of Education. Here’s how that breaks down:
- Commercial insurers saved $206 billion
- Medicare saved $137 billion - an average of $2,672 per beneficiary
- Medicaid saved $102 billion
By therapeutic area, the biggest savings came from:
- Heart disease: $118.1 billion
- Mental health: $76.4 billion
- Cancer: $25.5 billion
These aren’t theoretical numbers. For someone taking a daily blood pressure pill, a generic can cut their monthly cost from $150 to $10. For a cancer patient on a targeted therapy, switching to a generic can drop a $10,000 monthly bill to under $500.

Why the Two Numbers Are So Different
The FDA’s $5.2 billion in 2022 and the AAM’s $445 billion in the same year aren’t contradictory - they’re measuring different things.
The FDA looks at what happens in the first year after a single generic is approved. If that drug was selling for $1,000 per month and the generic drops it to $50, and 100,000 people switch, that’s $540 million saved in a year - just from that one drug.
The AAM looks at every generic drug being used right now - thousands of them - and compares what people actually paid versus what they would have paid if all those drugs were still brand-name. That’s why the total is so much higher. The FDA tracks the spark. The AAM measures the whole fire.
Who Benefits the Most?
It’s not just insurers and pharmacies that save money. Patients do too - but not always as much as you’d expect.
On average, a generic prescription costs $6.97 out of pocket. Ninety-two percent of generic prescriptions are filled for under $20. That’s a massive win for people without insurance or those with high deductibles.
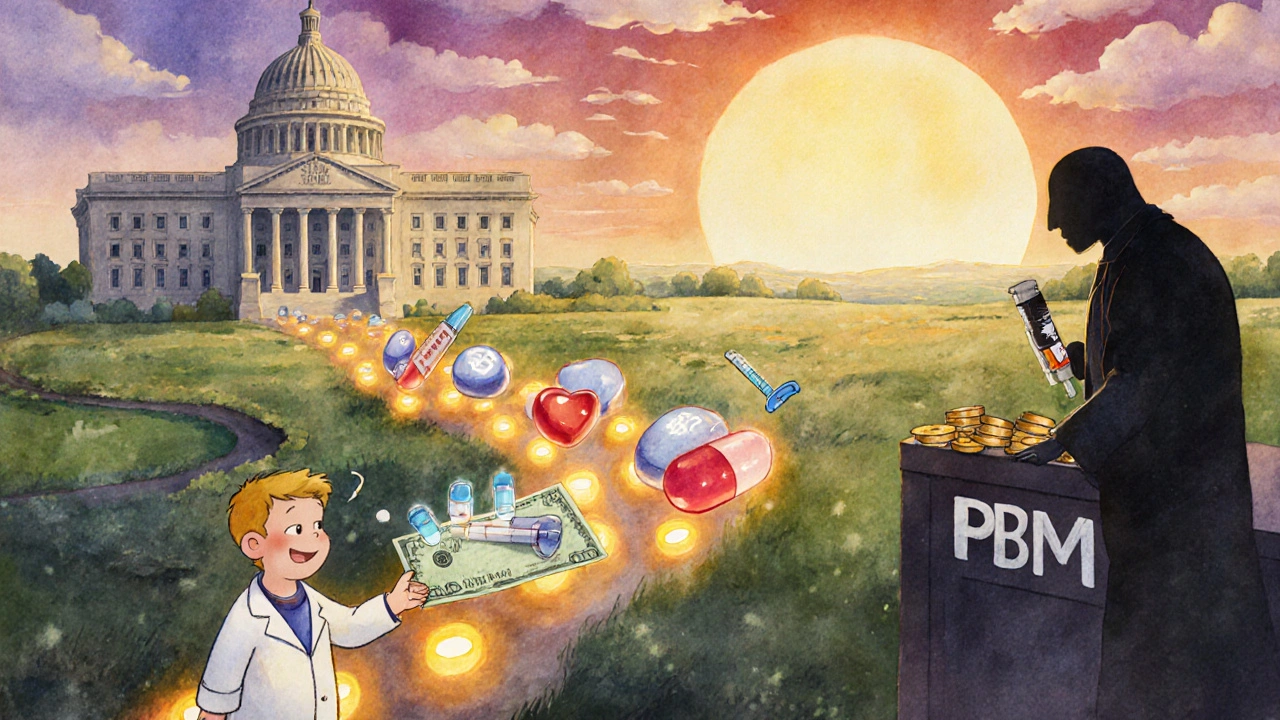
But here’s the catch: savings don’t always reach the patient. Pharmacy Benefit Managers (PBMs) negotiate rebates with drugmakers. When a generic is approved, the brand company often pays a rebate to the PBM to keep the drug on the formulary. That rebate doesn’t go to the patient - it goes to the middleman. A 2023 Senate Finance Committee report found that only 50-70% of the savings from generics actually make it to the consumer’s pocket.
State Medicaid programs see the clearest benefits. California’s Medi-Cal program saved $23.4 billion in a single year from generics. Alaska, with a much smaller population, still saved $354 million. The scale matches the population - but the impact is just as real.
The Bigger Picture: Generics Are the Backbone of Affordable Care
Generics make up 90% of all prescriptions filled in the U.S. - but they account for only 13.1% of total drug spending. That’s the power of competition.
The Hatch-Waxman Act of 1984 created the modern generic approval system. Back then, the FDA expected $1 billion in annual savings. Today, that number is over $400 billion. The system works - but it’s under pressure.
Brand-name companies are using legal tactics to delay generic entry: patent thickets, evergreening, and REMS (Risk Evaluation and Mitigation Strategies) that restrict access to samples needed for testing. The FDA’s 2023 Drug Competition Action Plan is trying to crack down on these delays.
Also, newer drugs - especially biologics - are harder and more expensive to copy. Biosimilars (the generic version of biologics) have only been around since 2015. As of August 2024, the FDA had approved 59 biosimilars. Their savings are still small compared to traditional generics, but they’re growing fast.
What’s Next?
Looking ahead, the pipeline is strong. Dozens of blockbuster drugs will lose patent protection between 2025 and 2030, including the arthritis drug Humira, the psoriasis drug Stelara, and the migraine drug Emgality. Each one could save billions.
By 2033, U.S. generic drug revenue is projected to hit $131.8 billion. That doesn’t mean drug companies are making more - it means more people are using cheaper versions. The real win? Lower costs for patients, fewer financial barriers to treatment, and a system that works better because of competition.
Generics aren’t just cheaper pills. They’re the reason millions of Americans can afford to take their medicine every day. And every year, the FDA’s approval list is a direct line from policy to pocketbook savings.
How are savings from generic drugs calculated by the FDA?
The FDA calculates savings by comparing the brand-name drug’s price before generic entry to the price after. They multiply the price difference by the number of prescriptions filled with the generic. They also account for the brand-name drug’s price drop after the generic enters the market. This is done for each new generic approval during the first 12 months after approval.
Why did generic savings drop in 2020 after being so high in 2019?
Savings depend on which brand-name drugs lose patent protection. In 2019, several high-revenue drugs like Januvia and Repatha went generic at the same time, driving savings to $7.1 billion. In 2020, fewer major drugs expired, so the total savings dropped to $1.1 billion. It’s not a decline in generic approvals - it’s a shift in which drugs are affected.
Do patients actually pay less when generics are approved?
Yes - but not always the full amount. The average generic copay is $6.97, and 92% of generics cost under $20. However, Pharmacy Benefit Managers (PBMs) often keep part of the savings as rebates. Studies show only 50-70% of the cost reduction reaches the patient directly.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs, like aspirin or metformin. Biosimilars are highly similar - but not identical - copies of complex biologic drugs, like insulin or Humira. Biosimilars are harder and more expensive to develop, which is why they’ve taken longer to enter the market. As of 2024, the FDA has approved 59 biosimilars.
How many generic drugs does the FDA approve each year?
The FDA approves between 600 and 750 generic drug applications each year. In 2022, it approved 742 applications. Not all of these are first-time generics - many are additional versions of drugs that already have generics on the market. The number of first generics (new entries into a previously brand-only market) varies from year to year, ranging from 40 to 80.
What’s the long-term impact of generic drug savings?
From 2014 to 2023, generics and biosimilars saved the U.S. healthcare system $3.1 trillion. That’s enough to cover the annual cost of Medicare for all Americans for over a decade. The AAM projects cumulative savings will reach $3.9 trillion by 2028. These savings keep medications affordable, reduce insurance premiums, and prevent patients from skipping doses due to cost.


Arup Kuri
November 26, 2025
So the FDA says generics save billions but you know who really gets rich? The PBMs. They’re the middlemen sucking down rebates while patients still struggle to afford insulin. This whole system is rigged. The brand companies pay them to keep prices high. It’s not about health-it’s about profit. And don’t even get me started on how they delay generics with patent crap.
Timothy Sadleir
November 27, 2025
The statistical disparity between the FDA’s first-year savings metric and the AAM’s aggregate annual savings is not indicative of an inconsistency in measurement, but rather a reflection of temporal and compositional variance in pharmaceutical market dynamics. The former captures discrete market shocks upon patent expiration; the latter quantifies the compounding fiscal impact of sustained market penetration across thousands of therapeutic agents. One is an event horizon; the other, a steady-state equilibrium.
Srikanth BH
November 28, 2025
This is actually really encouraging news. It shows that when we let competition work, people win. Generics aren’t just cheaper-they’re life-changing for so many families. I know someone who switched from brand-name blood pressure meds to generics and now they can actually afford their other prescriptions too. Small changes add up. Keep pushing for more approvals!
Jennifer Griffith
November 28, 2025
wait so generics are like 90% of rx’s but only 13% of spending?? that’s wild. so why do i still get billed like $40 for my zoloft? someone’s gettin rich off this and it ain’t me 😑
Kimberley Chronicle
November 30, 2025
The structural efficiency of the generic ecosystem is profoundly underappreciated. The Hatch-Waxman framework created a regulatory arbitrage that incentivized market entry without requiring redundant clinical trials. This resulted in an unprecedented reduction in marginal cost per therapeutic unit. The 90% market penetration rate with 13.1% expenditure share demonstrates a near-perfectly competitive equilibrium-something rarely observed in pharmaceutical markets. The real challenge now lies in extending this model to biosimilars, where regulatory and manufacturing complexity remains a barrier.
Karen Willie
December 2, 2025
I’ve seen this firsthand. My mom takes six different meds. Four are generics. She used to skip doses because of the cost. Now she takes them all. No drama. No panic. Just better health. It’s not glamorous, but this is what real healthcare reform looks like-quiet, steady, and life-saving.
Jefriady Dahri
December 2, 2025
Bro this is why I love science and policy working together 🙌 The FDA doesn’t just approve pills-they’re saving lives every single day. And yeah, PBMs are sketchy but at least we’re moving in the right direction. More generics = more people alive. That’s the win. Keep pushing for biosimilars too, they’re next big thing!
Sharley Agarwal
December 2, 2025
PBMs are thieves. They’re stealing from patients. This whole system is a scam.
Roscoe Howard
December 4, 2025
While the data presented is statistically sound, one must consider the broader geopolitical context. The United States, as the world’s largest pharmaceutical market, bears the burden of R&D funding. The erosion of brand-name pricing through aggressive generic competition undermines the very engine that drives innovation. One cannot have affordable drugs without first having drugs to afford. The balance is delicate.
Shirou Spade
December 5, 2025
It’s fascinating how a simple legal framework from 1984-Hatch-Waxman-became the quiet revolution that reshaped American healthcare. It wasn’t a protest, not a law passed in outrage, but a quiet compromise: let competition in, and the market will do the rest. And it did. The real tragedy isn’t the rebates or the PBMs-it’s that we’ve forgotten how powerful simplicity can be. We overcomplicate everything now. Maybe we just need to trust the system again.
Patricia McElhinney
December 6, 2025
the fda is just a puppet of big pharma. they approve generics when it’s convenient. look at humira-held up for years. and don’t get me started on how they let companies game the system with fake patents. this is all corruption. and the media never talks about it. why? because they’re paid off too.
Dolapo Eniola
December 7, 2025
Y’all in US think you got it bad? In Nigeria, we pay full price for brand drugs or go without. No generics. No rebates. No PBMs. Just God and hope. If you think your system’s broken, check out ours. At least you have a system. We got nothing. So stop complaining. Be grateful.
Agastya Shukla
December 8, 2025
Interesting how the FDA’s first-year savings metric correlates with the concentration of patent expirations in specific therapeutic classes. The 2019 spike wasn’t just volume-it was a convergence of high-ATC-class drugs (C10AA, A10BJ) with massive volume utilization. The 2022 rebound aligns with cardiovascular and respiratory agents (R03AK, R03BA). This suggests that the marginal savings per approval is non-linear and heavily dependent on baseline drug cost and patient prevalence. A useful predictive model could be built using patent cliff data and utilization metrics.