Every year, over 1.3 million people in the U.S. end up in the emergency room because of medication mistakes. Many of these aren’t caused by doctors or pharmacists-they happen at home. You take your pills, you think you’re doing it right, but something goes wrong. Maybe you mixed up your pills. Maybe you took them with the wrong drink. Maybe you didn’t realize the label changed. These aren’t rare mistakes. They’re common-and they’re preventable.
Rule 1: Know the Right Patient
It sounds obvious, but taking someone else’s medicine-or having someone else take yours-is one of the most dangerous things you can do. Even if you both have the same condition, your body reacts differently. Your weight, kidney function, age, and other medications all change how a drug works. Hospitals use two identifiers-like your name and date of birth-to confirm who gets what. At home, you need to do the same. Always check the name on the bottle against your ID. If you’re helping an elderly parent or child, make sure you’re giving the right person’s pills. Don’t rely on bottle shape, color, or where you left it on the counter. Keep each person’s meds in separate containers. Label them clearly. If you share a medicine cabinet, use locked boxes or locked drawers. One wrong pill can cause a hospital trip-or worse.Rule 2: Confirm the Right Drug
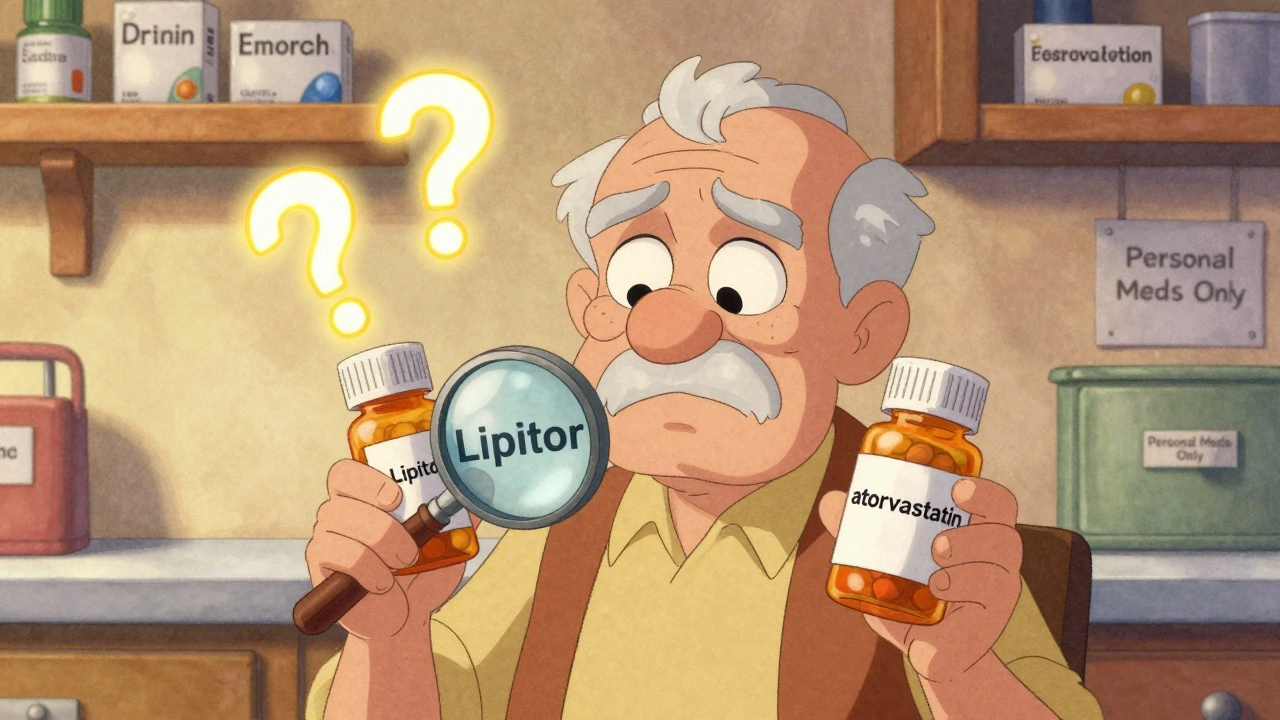
There are hundreds of drugs that look or sound alike. Insulin and heparin. Zyrtec and Zoloft. Clonazepam and clonidine. These aren’t typos-they’re real mix-ups that happen every day. The Institute for Safe Medication Practices says look-alike and sound-alike drugs cause about 25% of all medication errors. Always read the generic name on the label, not just the brand. If your prescription changed from “Lipitor” to “atorvastatin,” don’t assume it’s the same thing unless you check. When you pick up a refill, compare the pill to the last one. Does it look different? Is the imprint code changed? Is the color off? Don’t be afraid to ask the pharmacist: “Is this the same medicine I got last time?” If it doesn’t match what you expect, stop. Don’t take it. Call your doctor. A small difference in pill appearance can mean a big difference in effect.Rule 3: Get the Right Dose
Dosing isn’t one-size-fits-all. A 70-year-old with kidney issues needs less of some drugs than a 30-year-old. Children need doses based on weight-not age. Even small mistakes can be deadly. One common error? Confusing “mg” (milligrams) with “mcg” (micrograms). That’s a 1,000-fold difference. Insulin, thyroid meds, and blood thinners like warfarin are especially dangerous if dosed wrong. Always use the measuring tool that comes with the medicine-never a kitchen spoon. A teaspoon holds different amounts depending on the spoon. Use the syringe or cup provided. If your doctor changes your dose, write it down. Don’t rely on memory. Keep a list of all your meds, including doses, and update it every time something changes. If you’re unsure, call your pharmacist. They’re trained to catch dosing errors before they happen.
Rule 4: Use the Right Route
Taking a pill orally is not the same as injecting it. Swallowing a patch meant for your skin can be fatal. Putting eye drops in your ear can cause infection. Some meds are designed to dissolve under the tongue-chewing them ruins their effect. Always read the instructions. If it says “for oral use,” don’t crush it and mix it into food unless your doctor or pharmacist says it’s okay. Some pills are time-released. Crushing them can release the whole dose at once. That’s how overdoses happen. If you have trouble swallowing pills, ask your doctor if there’s a liquid form. Don’t assume that breaking a pill in half is safe-some are coated for a reason. If you’re given an injection, make sure you know how to use it. Ask for a demonstration. Watch a video from your pharmacy. Don’t guess. One wrong route can turn a helpful drug into a life-threatening one.Rule 5: Take It at the Right Time
Timing matters. Some meds work best on an empty stomach. Others need food to be absorbed. Blood pressure pills taken at night can lower your pressure too much while you sleep. Antibiotics taken too far apart lose effectiveness. Chemo pills often need to be taken within 15 minutes of the same time every day. Set phone alarms. Use a pill organizer with days and times labeled. If you miss a dose, don’t just double up. Check the label or call your pharmacist. For time-sensitive drugs, being 30 minutes early or late can make a difference. If you’re on five or more meds, schedule a medication review with your pharmacist every three months. They can help you sort out what to take when-and what might be interacting. Many seniors skip doses because they’re confused. That’s not laziness-it’s a system failure. You don’t have to remember everything. Use tools. Ask for help. Your health depends on consistency.What’s Missing from the Five Rules?
The Five Rights-right patient, drug, dose, route, time-are the foundation. But they’re not the whole picture. You also need to know the right reason. Why are you taking this? Is it for pain? For high blood pressure? For infection? If you don’t know, you can’t tell if it’s working. You also need to know the right response. Are you feeling better? Worse? Are you dizzy, nauseous, or having unusual bruising? These are signs something’s off. And don’t forget right documentation. Keep a written or digital list of everything you take, including vitamins and supplements. Bring it to every appointment. Finally, right education matters. If you don’t understand side effects or interactions, you’re flying blind. Ask your pharmacist: “What should I watch for?” “What should I avoid?” “What happens if I miss a dose?” Don’t be shy. These questions save lives.
Real-World Tips for Home Use
- Keep a list: Write down every medication, dose, and time. Update it every time something changes. Use your phone or a notebook-just keep it handy.- Use a pill organizer: Weekly or daily boxes with time slots help prevent double-dosing or skipping.
- Check expiration dates: Old pills lose potency. Some become toxic. Toss anything past its date.
- Read the label every time: Even if you’ve taken it for years. Labels change.
- Ask questions: If something seems off, speak up. Your pharmacist is your best ally.
- Use good lighting: Many errors happen because people can’t read small print. Use a lamp when taking meds at night.
- Do a brown bag review: Once a year, bring all your meds-bottles, supplements, OTCs-to your doctor or pharmacist. They’ll spot duplicates, interactions, and expired drugs you forgot about.
When to Get Help
If you’ve ever taken the wrong pill by accident, skipped doses because you were confused, or felt side effects you didn’t expect, you’re not alone. But you don’t have to handle it alone. Talk to your pharmacist. Ask for a medication therapy management (MTM) session-it’s free with most insurance. Use apps like Medisafe or MyTherapy to track doses and get reminders. If you’re caring for someone else, make sure they’re not hiding confusion out of embarrassment. Medication safety isn’t about being perfect. It’s about being aware, asking questions, and using tools to reduce risk. You’re not failing if you make a mistake. You’re failing if you don’t learn from it.What should I do if I take the wrong medication?
Stop taking it immediately. Call your pharmacist or poison control at 1-800-222-1222. Do not wait for symptoms. Even if you feel fine, some reactions take hours to show. Have the pill bottle ready when you call-they’ll need the name, dose, and how much you took. If you’re dizzy, having trouble breathing, or losing consciousness, call 911.
Can I crush my pills if I have trouble swallowing them?
Only if your doctor or pharmacist says it’s okay. Many pills are designed to release slowly. Crushing them can cause too much medicine to enter your system at once. Time-release tablets, capsules with beads, and coated pills should never be crushed. Ask for a liquid version instead. Some pharmacies can compound medications into easier-to-take forms.
Why do some meds need to be taken with food and others on an empty stomach?
Food can change how your body absorbs medicine. Some drugs need fat to dissolve properly-like certain antibiotics or cholesterol meds. Others can irritate your stomach if taken without food. Some are blocked by food and won’t work if taken with a meal. Always follow the label. If it says “take on an empty stomach,” wait at least one hour before eating or two hours after. If it says “take with food,” eat something light-like crackers or toast.
Is it safe to take expired medication?
Most expired meds aren’t harmful, but they may not work as well. Antibiotics, insulin, and epinephrine can become ineffective or even dangerous after expiration. The FDA says to throw out any medication past its date unless it’s part of an emergency stockpile. For chronic conditions, don’t risk it. Replace expired meds. If cost is an issue, ask your pharmacy about discount programs or generic alternatives.
How do I know if my meds are interacting with each other?
Talk to your pharmacist. They check for interactions every time you pick up a new prescription. Common dangerous combos include blood thinners with NSAIDs (like ibuprofen), statins with grapefruit juice, and antidepressants with certain cold meds. Keep a full list of everything you take-including vitamins, herbs, and OTC drugs. Even natural supplements can interfere with prescription meds. Don’t assume something is safe because it’s “natural.”

Sheldon Bird
December 12, 2025
This is the kind of post that makes me wanna hug my grandma and help her sort her pillbox. Seriously, I didn’t realize how many little things can go wrong until I read this. 😊
Karen Mccullouch
December 14, 2025
Of course the government doesn’t want you to know how easy it is to mess up meds. Big Pharma’s got a billion-dollar gravy train riding on confusion. 🤡
Michael Gardner
December 16, 2025
Wait, so you’re telling me I shouldn’t just take whatever’s in the little white pill bottle I found on the counter? What’s next, don’t drink random liquids from unlabeled bottles?
Willie Onst
December 16, 2025
I love how this post doesn’t just list rules-it gives you the why behind them. It’s like someone sat down with you over coffee and said, ‘Hey, here’s how to not accidentally poison yourself.’ 🙌
My aunt used to mix her blood pressure meds with her arthritis pills because they looked alike. She didn’t realize until she passed out at the grocery store. This post? It’s the kind of thing that could’ve saved her. Thanks for writing it.
Tyrone Marshall
December 18, 2025
One thing this doesn’t mention enough: the role of caregivers. I’ve seen so many elderly folks who are terrified to ask questions because they don’t want to seem ‘stupid.’ But the truth? They’re the ones keeping the whole system running. If you’re helping someone manage meds, don’t just hand them the bottle-sit with them. Read the label together. Set alarms. Make it a ritual. Safety isn’t a checklist. It’s a relationship.
Also, if you’re using a pill organizer, label the days with words, not just symbols. My uncle mixed up Wednesday and Friday because he couldn’t read the icons. He took his anticoagulant twice in one day. That’s not negligence-that’s design failure.
Emily Haworth
December 20, 2025
They’re hiding something. Why do ALL the pills look the same? Why don’t they use colors or shapes that match the condition? I bet the FDA’s in bed with the drug companies. And why do they still use tiny print? It’s intentional. They want you to mess up. 🕵️♀️💊
Tom Zerkoff
December 21, 2025
While the Five Rights framework is foundational, it is imperative to recognize that medication safety is a systems-level challenge. The burden of verification is disproportionately placed on the patient, who often lacks the clinical literacy required to interpret pharmaceutical labeling accurately. A robust intervention strategy must include standardized visual coding, mandatory pharmacist-led counseling at each dispensing event, and integration of electronic health records with automated patient alerts. Furthermore, the absence of mandatory patient education modules in primary care settings constitutes a critical gap in public health infrastructure.
Keasha Trawick
December 23, 2025
OMG I just realized I’ve been crushing my mom’s extended-release pills because she said they ‘taste like chalk.’ 😳 I thought it was fine! Now I’m Googling ‘what happens if you crush amlodipine’ and my heart’s racing. Thanks for the wake-up call. I’m calling her pharmacist right now. 🙏
Webster Bull
December 23, 2025
just check the bottle. every time. even if you’ve taken it for 10 years. labels change. you dont wanna be that guy who took his neighbor’s heart med because it looked like his own. 💀