Understanding Duchenne Muscular Dystrophy
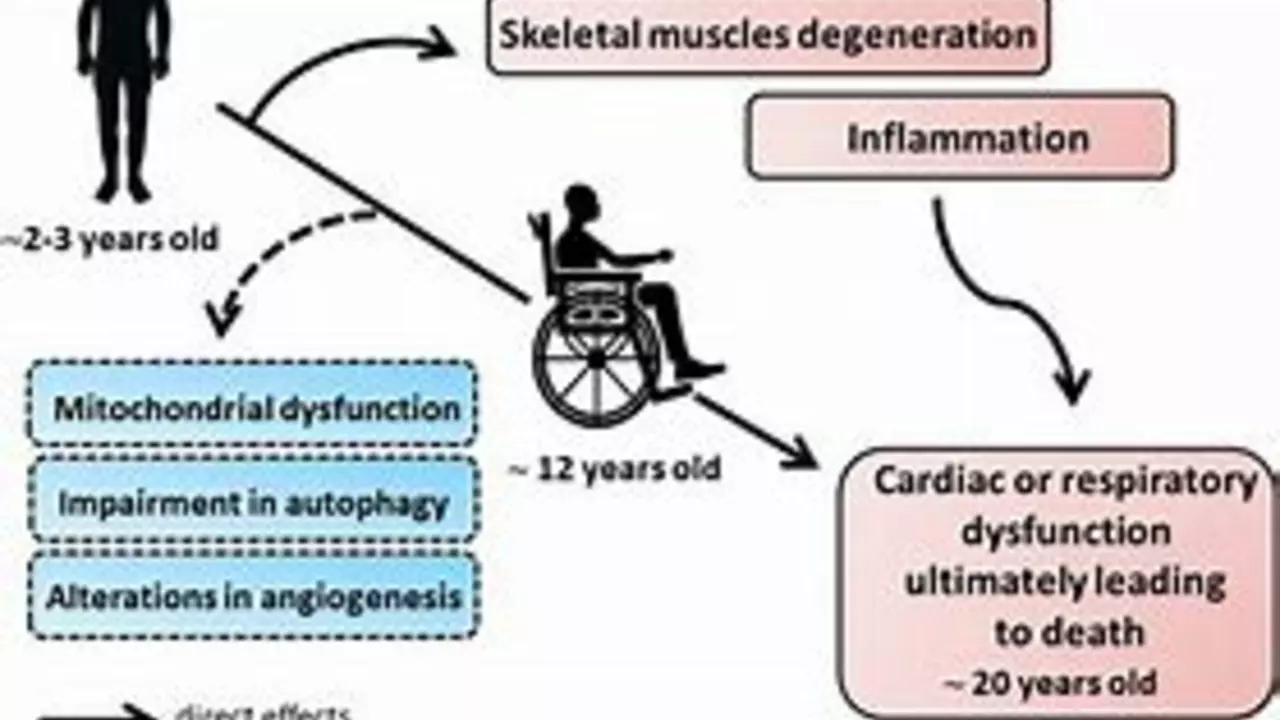
Before we delve into the complexities of preparing for end-of-life care with Duchenne Muscular Dystrophy (DMD), it's crucial to understand what this disease is. Duchenne Muscular Dystrophy is a rare genetic disorder that primarily affects boys. It results in progressive muscle weakness and degeneration, eventually affecting the heart and lungs. It's a condition that starts early in life but its consequences become more severe and apparent as the person ages.
Recognizing the Progression of Duchenne Muscular Dystrophy
The progression of DMD is gradual and varies from person to person. However, understanding the typical progression can help in planning for the future. Initially, symptoms may include difficulty in walking, running or climbing stairs. As the disease progresses, individuals may need a wheelchair for mobility. Eventually, DMD affects the heart and lungs, leading to serious health complications.
Initiating Conversations about End-of-Life Care
Discussing end-of-life care is never easy, especially when it involves a loved one with DMD. However, these conversations are essential to ensure that the person's wishes are respected and their comfort maximized. Start discussing these topics early, and encourage open and honest communication. Remember, it's okay to have multiple conversations over time as it can be an overwhelming topic.
Planning for Medical Care
Medical care planning is a crucial aspect of end-of-life care. It involves understanding the potential health complications related to DMD and deciding on the appropriate interventions. This could range from decisions on respiratory support to cardiac care. It's essential to involve the person with DMD, their family, and their healthcare team in these discussions.
Understanding Palliative Care Options
Palliative care plays a vital role in managing the symptoms and improving the quality of life for individuals with DMD. This type of care focuses on pain management, emotional support, and other therapies that can enhance comfort. It's important to understand that palliative care can be utilized at any stage of the disease and is not just for the end-of-life stage.
Exploring Hospice Care
When the disease has progressed to a severe stage, hospice care might be the right choice. Hospice care provides comprehensive comfort care, including pain management, emotional and spiritual support, and help for families. It's provided by a team of professionals who are experts in end-of-life care.
Consideration for Legal and Financial Planning
Legal and financial planning becomes crucial when preparing for end-of-life care. This includes making a will, setting up a trust, or assigning power of attorney. It's also important to look into insurance coverage, disability benefits, and other financial resources that can help cover the costs of care.
Emotional and Psychological Support
Living with DMD or caring for someone with the disease can be emotionally challenging. It's vital to ensure that emotional and psychological support is available, whether it's through counseling, support groups, or other resources. This aspect of care is as important as the physical and medical care.
The Role of Family and Caregivers
The role of family and caregivers in the care of a person with DMD cannot be understated. They provide the day-to-day care, emotional support, and often act as advocates for the person with DMD. It's important for them to be well-informed, supported, and included in all decision-making processes.
Living Life to the Fullest
Despite the challenges that come with DMD, it's important to remember that life can still be lived to its fullest. This means focusing on what brings joy and fulfillment, whether it's spending time with loved ones, pursuing hobbies, or simply enjoying the moment. End-of-life care is not just about managing the disease, but also about enhancing the quality of life.

Jacqui Bryant
July 26, 2023
Taking the first step toward planning can feel overwhelming but it’s also a way to keep control. Simple daily check‑ins with the care team can build confidence. Remember that small wins add up and keep the focus on quality of life.
Paul Luxford
July 28, 2023
I appreciate the calm tone here and value the respectful boundaries set around this conversation.
Nic Floyd
July 29, 2023
The multidisciplinary approach to DMD end‑of‑life planning integrates palliative oncology cardiopulmonary physiotherapy and advanced directives within a patient‑centered framework.
The care continuum leverages interoperable health records to synchronize respiratory support protocols across acute and home settings.
Proactive cardiac monitoring using echocardiographic strain imaging can preempt decompensation events.
Genetic counseling services are essential for familial risk stratification and psychosocial adaptation.
Integration of telemedicine platforms streamlines multidisciplinary conferences and reduces caregiver travel burden.
Evidence‑based guidelines suggest initiating non‑invasive ventilation before nocturnal hypoxia thresholds are breached.
Pharmacologic adjuncts such as corticosteroid regimens must be balanced against metabolic side effects.
Legal considerations include durable power of attorney for health care and early will drafting to alleviate future uncertainties.
Financial navigation tools like disability benefit calculators help families allocate resources efficiently.
Psychosocial support can be delivered via peer‑led support groups that harness shared lived experience.
Spiritual care providers can offer narrative meaning‑making sessions that align with personal belief systems.
Advance care planning documents should be revisited quarterly to reflect disease trajectory changes.
Hospice eligibility criteria focus on symptom burden rather than chronological disease stage.
Quality‑of‑life metrics such as the Pediatric Quality of Life Inventory guide therapeutic priorities.
Caregiver resilience programs incorporate mindfulness training and respite scheduling.
Ultimately a coordinated care model empowers patients and families to navigate the complex DMD journey 😊.
Johnae Council
July 30, 2023
Look, the article hits the usual checklist but skips the gritty realities families face daily. Some of the advice feels like a corporate brochure not a real lived experience.
Manoj Kumar
July 31, 2023
Oh sure just sprinkle a little optimism on a situation that practically screams mortality and everything magically aligns. In the grand theater of existence even DMD has its own tragic comedy.
Hershel Lilly
August 1, 2023
Could there be more data on how early hospice enrollment impacts long‑term emotional outcomes for caregivers?
Carla Smalls
August 2, 2023
Staying proactive and celebrating each milestone no matter how small makes the journey richer for everyone involved.