PAD Treatment: What Works, What to Avoid, and How to Stay Safe
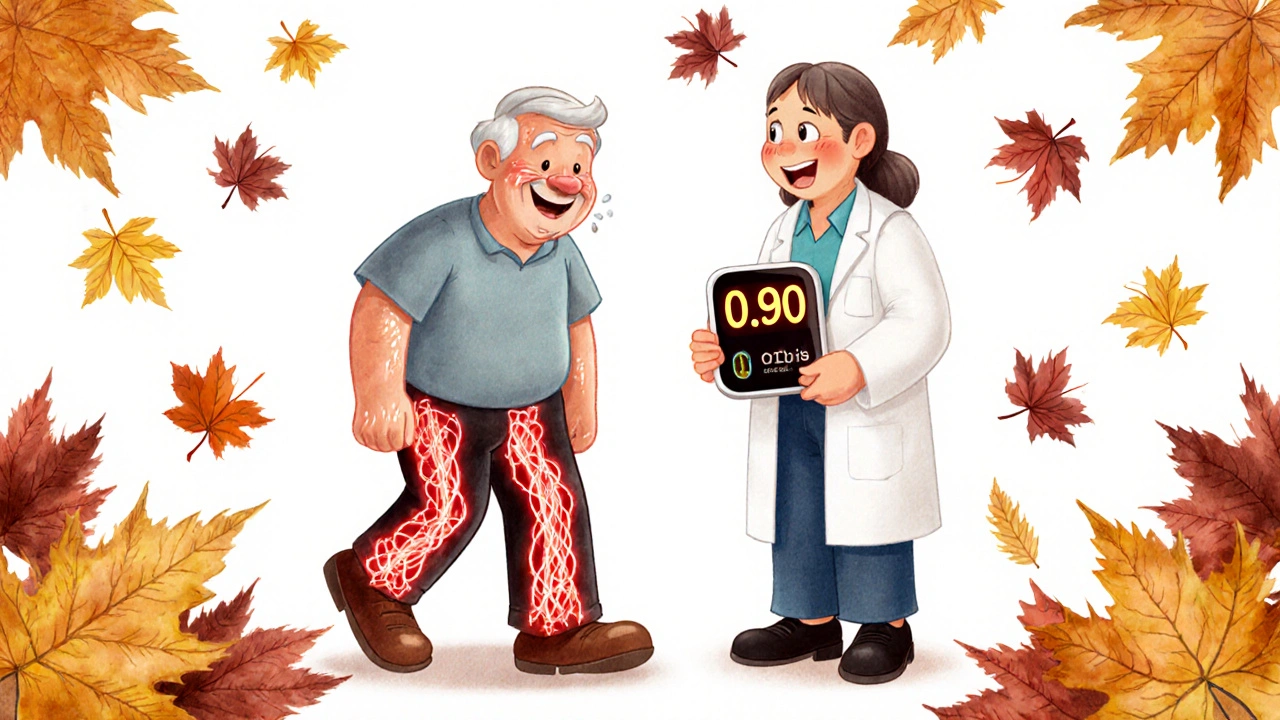
When you have peripheral artery disease, a condition where narrowed arteries reduce blood flow to your limbs, often causing leg pain when walking. Also known as PVD, it’s not just a aging issue—it’s a warning sign your heart and arteries are under stress. If you’re walking slower, getting cramps in your calves, or noticing your feet feel colder than usual, you’re not just getting older—you might have PAD treatment needs that can’t wait.
PAD treatment isn’t one-size-fits-all. Some people think popping a pill is enough, but the most effective approach combines medication, movement, and lifestyle changes. Walking programs, for example, are proven to improve blood flow better than many drugs. Studies show that walking 30 minutes, five days a week, can double your pain-free walking distance in just 12 weeks. That’s not magic—it’s biology. Your muscles learn to use oxygen better, and your body grows tiny new blood vessels to bypass the blockages.
Medications play a role too. antiplatelet drugs, like aspirin or clopidogrel, stop blood clots from forming in narrowed arteries—and skipping them can raise your risk of heart attack or stroke. But not all meds are safe for everyone. If you’re on ACE inhibitors, used for high blood pressure and kidney protection, you need to watch your potassium levels. Too much from bananas, potatoes, or salt substitutes can turn dangerous when combined with these drugs. And if you’re taking pain relievers like diclofenac, a common NSAID found in Voveran, you’re risking higher blood pressure and fluid retention—exactly what PAD patients should avoid.
What you eat matters more than you think. Processed foods, sugar, and trans fats make arteries stiffer. Simple swaps—like swapping white bread for whole grains, or soda for water—can slow progression. And don’t ignore smoking. Quitting is the single most effective thing you can do to stop PAD from getting worse. It’s not about willpower—it’s about protecting your blood vessels from toxins that wreck their lining.
There’s also a hidden risk: some people with PAD end up on multiple meds that clash. Anticholinergics, used for bladder issues or GI spasms, can cause confusion or urinary retention—especially in older adults. And if you’re taking statins for cholesterol, muscle pain might be a sign you need a dose check. It’s not just about treating the blockage—it’s about managing the whole system.
Below, you’ll find real, practical guides that cut through the noise. Learn how to safely restart meds after a break, avoid dangerous food-drug combos, understand why generic pills sometimes feel different, and how to monitor your kidney health if you’re taking creatine or ACE inhibitors. These aren’t theory pieces—they’re tools built by people who’ve been there. Whether you’re newly diagnosed or managing PAD for years, the right info can mean the difference between walking without pain… and ending up in the hospital.