Peripheral artery disease, or PAD, isn’t just about sore legs after walking. It’s a warning sign that your arteries are clogging up - not just in your legs, but possibly throughout your body. If you’re over 50, smoke, have diabetes, or high blood pressure, you’re at risk. And here’s the scary part: most people with PAD don’t even know they have it. Only about 20% of eligible patients get tested. That means millions are walking around with blocked arteries, unaware they’re one heart attack or stroke away from a life-changing event.
What Does PAD Actually Feel Like?
The classic symptom is claudication - cramping or tiredness in your calves, thighs, or buttocks that shows up when you walk and disappears when you stop. It’s not just being out of shape. It’s your muscles screaming for more blood. You might notice you can only walk a block or two before needing to rest. After a few minutes, you’re fine again. That’s claudication. About 10% of PAD patients have this clear sign. The rest? They might just think they’re getting older. But PAD doesn’t always announce itself with pain. Some people get cold feet that never warm up, even in a heated room. Others notice their leg hair has thinned out or stopped growing. Their skin looks shiny, dry, or pale. Toenails may thicken and stop growing. In men, erectile dysfunction can be an early red flag - up to 75% of male PAD patients experience it. These aren’t random aging changes. They’re signs your blood flow is failing. The worst-case scenario is critical limb ischemia. This is when pain hits even when you’re lying still - especially at night. Wounds on your feet won’t heal. You might see black spots on your toes. This is an emergency. Without treatment, amputation becomes likely. About 1% of PAD patients reach this stage, but when they do, nearly half lose a limb within a year if nothing’s done.How Do Doctors Know It’s PAD?
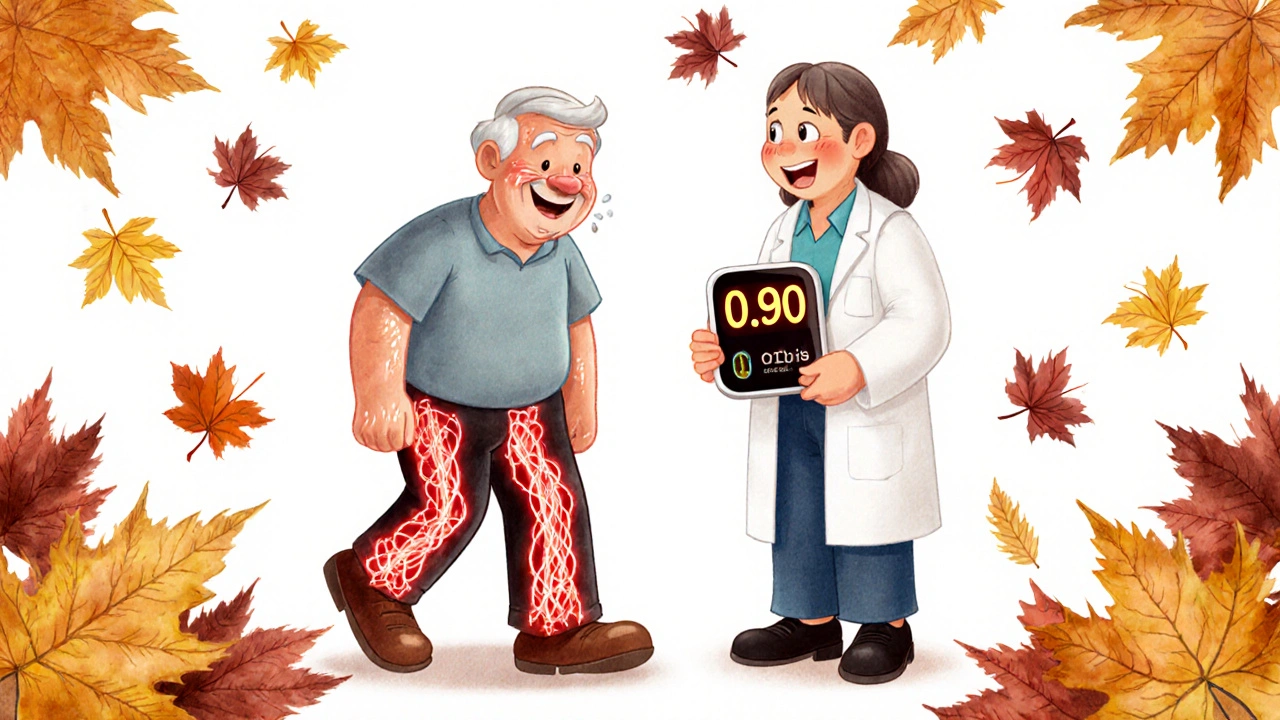
The first test is simple, painless, and takes less than 10 minutes. It’s called the ankle-brachial index, or ABI. They measure your blood pressure in your arm and then at your ankle. If the ankle number is less than 90% of the arm number, you have PAD. An ABI below 0.90 confirms it in 95% of cases. It’s that accurate. And yet, most doctors don’t order it unless you’re over 65, have diabetes, or smoke. If your ABI is borderline or you have diabetes (where arteries can be stiff and give false readings), they’ll check your toe pressure instead. That’s the toe-brachial index, or TBI. A TBI under 0.70 means you’ve got significant blockage. Beyond that, they might use ultrasound. It shows exactly where the blockage is and how fast blood is moving. It’s non-invasive, no needles, no radiation. For more detail, they’ll use a CT angiogram or MRI. These create 3D pictures of your arteries. They’re not perfect - they need contrast dye, which can be risky for people with kidney problems - but they’re powerful tools. The gold standard? Catheter angiography. A thin tube is threaded up from your groin to your legs, dye is injected, and real-time X-rays show every blockage. It’s invasive, expensive, and carries small risks. But if surgery is being considered, they need this level of detail.What Happens After Diagnosis?
The goal isn’t just to fix your legs. It’s to keep your heart and brain safe. PAD means your whole body’s arteries are likely damaged. People with PAD are 3 to 5 times more likely to have a heart attack or stroke. So treatment is two-pronged: relieve your symptoms and protect your life. The first step? Stop smoking. Seriously. If you keep smoking, your risk of amputation goes up eightfold. Your chance of dying within five years triples. Quitting is the single most effective thing you can do. Next: exercise. Not just walking around the house. A supervised walking program - 30 to 45 minutes, three to five times a week - can double your walking distance in just 12 weeks. It sounds counterintuitive: you walk until it hurts, rest, then walk again. But this trains your body to use oxygen better and grow new tiny blood vessels. It’s as effective as some surgeries for improving mobility.
Medications That Actually Work
You’ll likely be on at least three types of meds. First, antiplatelets. Aspirin (81 mg daily) helps. But clopidogrel (75 mg daily) is better - it cuts your risk of heart attack, stroke, or death by 20% more than aspirin. You don’t need both. One is enough. Second, statins. Not just to lower cholesterol. To stabilize plaque. All PAD patients should be on a high-dose statin, no matter their cholesterol level. Studies show they reduce major heart events by 25-30%. The goal? LDL under 70 mg/dL. Third, cilostazol. This pill helps you walk farther without pain. It increases walking distance by 50-100%. But it’s not for everyone. If you have heart failure, avoid it. Side effects include headaches and rapid heartbeat. For high blood pressure, aim for under 130/80. For diabetes, keep HbA1c under 7%. These aren’t optional. They’re part of the treatment plan.When Procedures Are Needed
If walking and meds aren’t enough, or if you’re in pain at rest, you might need a procedure. Angioplasty is the most common. A tiny balloon is inflated inside the blocked artery to open it. A stent - a small metal mesh tube - is often left behind to keep it open. For short blockages, this works in 90% of cases. But arteries can re-narrow over time. Atherectomy removes the plaque physically. It’s useful when arteries are full of calcium. Success rates are around 75%. It’s less common but growing in use. Bypass surgery is the old-school option. A vein from your leg or a synthetic tube is grafted around the blocked section. It lasts longer - 80% of vein grafts stay open after five years. But it’s major surgery. Recovery takes weeks. The choice depends on where the blockage is, how long it is, your overall health, and your goals. For many, a combination of exercise and medication is enough. For others, a procedure gives back their life.
The Big Picture: Why This Matters
PAD isn’t just a leg problem. It’s a full-body emergency. The five-year death rate for PAD patients is 30-40%. That’s worse than many cancers. And it’s preventable. Screening is key. If you’re over 65, or over 50 with diabetes or smoking history, ask for an ABI test. It’s free or low-cost in most clinics. If you’re younger but have multiple risk factors - high blood pressure, obesity, family history - get screened anyway. There’s also a huge gap in care. Black and Hispanic patients are 30-40% less likely to get revascularization, even when their disease is just as bad. That’s not just unfair - it’s deadly. New treatments are coming. Trials are testing blood-thinning drugs like rivaroxaban combined with aspirin to prevent limb complications. Stem cell therapy is being studied to grow new blood vessels in feet with non-healing wounds. And new imaging tools let doctors see plaque in microscopic detail, guiding more precise treatments. But none of that matters if you don’t know you have it. If you’re tired after walking, your feet are cold, or your toenails have stopped growing - don’t ignore it. Talk to your doctor. Get tested. Your legs - and your life - depend on it.What You Can Do Today
- Ask your doctor for an ankle-brachial index (ABI) test if you’re over 50 and smoke or have diabetes.
- If you smoke, quit. Call a quitline or ask for help. There’s no better investment in your future.
- Start walking - even if it hurts. Do 30 minutes, three times a week. Rest when you need to. Keep going.
- Take your meds as prescribed. Don’t skip statins or antiplatelets.
- Check your feet daily. Look for cuts, sores, color changes, or swelling. Treat even small wounds seriously.
Can peripheral artery disease be reversed?
Yes, in many cases. While damaged arteries won’t fully return to normal, plaque can stabilize, and blood flow can improve significantly. Lifestyle changes - quitting smoking, regular walking, and taking prescribed medications - can reduce blockages and prevent progression. Studies show that supervised exercise can increase walking distance by up to 200%. In some patients, symptoms disappear entirely.
Is PAD the same as heart disease?
PAD is a type of heart disease - specifically, a form of atherosclerosis that affects arteries outside the heart. But having PAD means your entire vascular system is at risk. People with PAD have the same high risk of heart attack and stroke as those with coronary artery disease. Treating PAD isn’t just about your legs - it’s about protecting your heart and brain.
Can you have PAD without any symptoms?
Absolutely. Up to 80% of people with PAD have no noticeable symptoms. They might feel fine walking, but their arteries are still narrowing. That’s why screening is so important, especially for people over 50 with risk factors like smoking, diabetes, or high blood pressure. Silent PAD is dangerous because it increases your risk of heart attack and stroke without warning.
Does walking hurt my legs if I have PAD?
Yes - but that’s normal and part of treatment. The pain, called claudication, happens because your leg muscles aren’t getting enough oxygen during activity. It’s not damage - it’s a signal. Walking through the pain (and resting when needed) trains your body to adapt. Over time, your muscles become more efficient, and you’ll walk farther before pain returns. Avoiding walking makes it worse.
What’s the difference between ABI and TBI?
ABI measures blood pressure at your ankle compared to your arm. It’s the standard test. But in people with diabetes or kidney disease, leg arteries can become stiff and give falsely high readings. That’s where TBI comes in - it measures pressure at your toe instead. A TBI under 0.70 confirms PAD when ABI results are unclear. TBI is more accurate for these groups.
Are there natural remedies for PAD?
There’s no proven natural cure. Supplements like ginkgo biloba or L-arginine have been studied, but none show consistent benefit. The only proven natural treatment is exercise - specifically, a structured walking program. Quitting smoking, eating a heart-healthy diet, and controlling blood pressure and sugar are also essential. Don’t rely on herbs or vitamins. Stick to science-backed treatments.
How often should I get checked if I have PAD?
If you’ve been diagnosed, see your doctor every 3 to 6 months for the first year. They’ll check your ABI, blood pressure, cholesterol, and foot health. After that, annual checkups are usually enough if things are stable. But if you develop new pain, sores, or color changes in your feet, call your doctor right away - don’t wait.
Can PAD lead to amputation?
Yes, but it’s preventable. Amputation usually happens only in advanced cases called critical limb ischemia - when you have pain at rest, non-healing wounds, or tissue death. With early diagnosis, proper medication, and timely revascularization, most people avoid amputation. The key is not ignoring early signs like cold feet, slow-healing sores, or loss of hair on your legs.

Allison Turner
November 28, 2025
Wow, another doctor post pretending they’re saving lives. I’ve seen this exact article three times this month. Everyone’s just scared of dying so they click on anything with ‘heart attack’ in the title. I’m 52, smoke a little, and my legs are fine. Stop scaring people.
Also, why is everyone suddenly obsessed with ABI tests? My cousin got one and they told him he had ‘borderline’ and now he’s on five meds and terrified to walk upstairs. He’s fine. He just needs to stop eating donuts.
Darrel Smith
November 28, 2025
Let me tell you something, folks. This isn’t just about legs. This is about the system failing you. You think they care if you live or die? No. They want you on statins for life. They want you to get that angioplasty so they can bill $30,000. And then you’re stuck on aspirin and clopidogrel forever because the system doesn’t want you cured-it wants you dependent.
I’ve seen it. My uncle had PAD. He quit smoking, walked every day, ate clean. They still wanted to cut him open. He refused. He’s alive at 82. No stents. No surgery. Just discipline. The medical industrial complex hates people like him. Because he didn’t need them. He needed willpower. And they don’t get paid for willpower.
Don’t let them turn your body into a profit center. Your legs aren’t broken. Your trust in doctors is.
And if you’re still smoking after reading this? You’re not just stupid. You’re complicit in your own destruction.
Aishwarya Sivaraj
November 29, 2025
My dad had PAD and no one knew until he got a sore on his toe that wouldn’t heal. We thought it was just old age. He was 68. By the time they tested him his ABI was 0.6. He almost lost his foot.
But he started walking every morning even when it hurt. He quit smoking cold turkey. Took his statin. Now he walks 3 miles without stopping. He says the pain isn’t gone but it’s different now. Like his body is learning to speak a new language.
If you’re reading this and you’re over 50 or have diabetes please please please ask for the ABI test. It’s free. It takes 5 minutes. It might save your leg. Or your life. I’m not exaggerating. I’ve seen what happens when you wait.
And if you think it’s just aging? It’s not. It’s your arteries screaming. Listen.
Also i forgot to mention my dad loves his morning tea and he still eats ice cream once a week. He’s not perfect. He’s just trying. And that’s enough.
you are not alone in this
Iives Perl
December 1, 2025
ABI tests are a scam. They’re funded by Big Pharma and the imaging companies. They want you scared so you’ll get the CT angiogram with contrast dye that ruins your kidneys. Then you need dialysis. Then you’re on Medicare. Then the government pays. It’s all connected.
My neighbor got the test. Then got the stent. Then got a stroke. Coincidence? I think not.
Walk barefoot on grass. Drink apple cider vinegar. Your body knows how to heal. The system just doesn’t want you to remember that.
Also the government is hiding the truth about PAD. Why do you think they don’t screen everyone? Because if everyone knew how common it is… well. Let’s just say the medical complex would collapse.
Wake up. 🚨
steve stofelano, jr.
December 2, 2025
It is with profound respect for the clinical rigor presented in this exposition that I offer my appreciation for the comprehensive elucidation of peripheral artery disease as a systemic manifestation of atherosclerotic burden. The delineation of diagnostic modalities, particularly the comparative utility of ABI versus TBI in diabetic populations, reflects a nuanced understanding of vascular pathophysiology that is all too often neglected in primary care settings.
Furthermore, the emphasis on supervised exercise as a therapeutic intervention of comparable efficacy to revascularization procedures represents a paradigmatic shift toward patient-centered, non-invasive management-a model I have advocated for in my own practice for over two decades.
I would only add that cultural and socioeconomic disparities in access to vascular care remain a moral imperative requiring urgent policy intervention, particularly in marginalized communities where screening rates remain unacceptably low.
Thank you for this vital contribution to public health literacy.
Savakrit Singh
December 3, 2025
India has the highest number of PAD patients in the world and yet we have less than 5% screening rate. Doctors here think it's 'just leg pain'. My uncle died because they didn't check his ABI. He was 59. Smoked. Diabetic. They told him to take painkillers.
Now I tell everyone I know: if you're over 50 and have sugar or smoke - get the test. It's 500 rupees. No insurance needed.
Also - statins are not optional. If your doctor says 'your cholesterol is fine so you don't need it' - find a new doctor. PAD isn't about cholesterol. It's about plaque. And plaque doesn't care if your LDL is 120 or 80. It only cares if you're not on a high-dose statin.
And yes - walking hurts. But it's better than losing your leg. 💪🩺
Cecily Bogsprocket
December 3, 2025
I know how scary this sounds. I’ve been there. My mom was diagnosed with PAD after she couldn’t walk to the mailbox without stopping. She cried for weeks. Thought she was going to lose her leg.
But she started walking. Just 10 minutes a day. Then 15. Then 30. She didn’t do it perfectly. Some days she skipped. Some days she was in too much pain. But she kept coming back.
Now she walks two miles. She says the pain isn’t gone, but it’s not the enemy anymore. It’s just a signal. Like a car’s check engine light.
If you’re reading this and you’re scared - I get it. But you’re not alone. And you don’t have to do this alone. Find a walking buddy. Call a support group. Talk to someone.
You don’t have to be perfect. You just have to show up.
And if you’re a smoker? I know quitting is hard. But it’s the most powerful thing you can do. I promise. I’ve seen it change lives.
Emma louise
December 4, 2025
Oh great. Another liberal health scare dressed up as ‘education’. Next they’ll tell us to wear masks while walking. Or that cold feet are a ‘government conspiracy’. This is why America’s dying - people believe everything they read on the internet. My grandfather smoked for 60 years, never had PAD, and died at 92 playing golf.
Stop weaponizing fear. Not everyone’s a walking time bomb. Some people are just… fine.
Also, why is this article pushing ‘cilostazol’? That’s a drug that costs $500 a month. Who’s getting rich off this? Not me.
Wake up. You’re being manipulated.
sharicka holloway
December 4, 2025
Hey. I just wanted to say - if you’re reading this because you’re worried about your legs, you’re not weird for being scared. I was there. I ignored my cold feet for a year. Thought it was just the heater being broken.
When I finally got the ABI test, I cried. Not because I had it - but because I realized I’d been so afraid to face it.
But here’s the thing: you don’t have to fix everything today. Just one thing. Maybe it’s walking for 10 minutes. Maybe it’s calling your doctor. Maybe it’s telling someone you’re scared.
You’re not broken. You’re not failing. You’re just human.
And you deserve to walk without pain.
I’m rooting for you.
Alex Hess
December 5, 2025
This is the kind of low-effort, clickbait pseudo-medical drivel that gives real science a bad name. ‘Up to 75% of male PAD patients experience ED’? So what? That’s not a diagnosis, that’s a correlation you found in a PubMed abstract. And ‘walking trains your body to grow new blood vessels’? That’s angiogenesis 101, not a miracle cure. This article reads like a med student’s first draft.
And don’t even get me started on the ‘screening for everyone over 50’ nonsense. You’re not a statistic. You’re not a risk factor. You’re a person. And if you’re asymptomatic, leave it alone. Overdiagnosis is a plague.
Also, why is this post promoting cilostazol? That drug has a 40% dropout rate due to side effects. Who’s paying for this propaganda?
Shubham Semwal
December 7, 2025
Let me break this down for you people who think this is just about walking. PAD isn’t a leg problem. It’s a death sentence you ignore until it’s too late. I’ve seen it. My brother had it. He ignored it because he ‘didn’t feel sick’. Then he got a toe ulcer. Then gangrene. Then amputation. Then a heart attack six months later.
Stop thinking this is about ‘being out of shape’. It’s about your arteries turning to concrete. And if you’re over 50 and smoke? You’re already in the danger zone. No exceptions.
And no - you can’t ‘boost circulation’ with ginkgo or garlic. That’s snake oil. The only thing that works is statins, quitting smoking, and walking until you want to cry. Then walking some more.
And if your doctor doesn’t order an ABI? Fire them. It’s the simplest test in medicine. If they don’t know it, they don’t know anything.
Sam HardcastleJIV
December 8, 2025
While the clinical utility of the ankle-brachial index is well established, one must interrogate the epistemological underpinnings of mass screening protocols. The assumption that asymptomatic individuals benefit from early detection presupposes a linear progression of disease - a model increasingly challenged by the heterogeneity of atherosclerotic phenotypes.
Moreover, the psychological burden of false positives in low-prevalence populations may outweigh the marginal gains in morbidity reduction. One wonders whether the push for universal ABI screening is driven more by liability mitigation than by patient outcomes.
That said, the emphasis on supervised exercise as first-line therapy remains a commendable deviation from the procedural-centric paradigm. One hopes this trend continues.
Mira Adam
December 9, 2025
They say PAD is silent. But I say it’s screaming. And we’re all too busy scrolling to hear it.
I used to think it was just old people. Then my 54-year-old cousin lost her foot because she thought ‘it’s just soreness’. She didn’t have diabetes. Didn’t smoke. Just… ignored it.
Now I look at my own feet every night. I walk. I take my pill. I don’t wait for pain. I don’t wait for a doctor to say ‘it’s probably nothing’.
Because the truth? It’s never nothing.
And if you’re reading this and you’re scared? Good. That means you’re still alive enough to care.
Miriam Lohrum
December 11, 2025
Interesting. I wonder if the emphasis on walking as therapy is really about cost containment. If you can get people to walk instead of operate, you save millions. But is that the right reason to promote it?
Also, why is there no mention of diet? Mediterranean diet has been shown to improve endothelial function. But this article skips it entirely. Odd.
Allison Turner
December 12, 2025
Wow. You guys are really into this. I still think it’s all fear porn. But hey, if walking helps, fine. I’ll walk to the fridge. That’s my daily cardio.
Also, I’m still smoking. And I’m still fine. Deal with it.