Postherpetic Neuralgia Relief Calculator
This calculator estimates potential pain reduction from massage therapy for postherpetic neuralgia (PHN). Based on research showing 30-35% average pain reduction with regular massage sessions.
Estimated Results
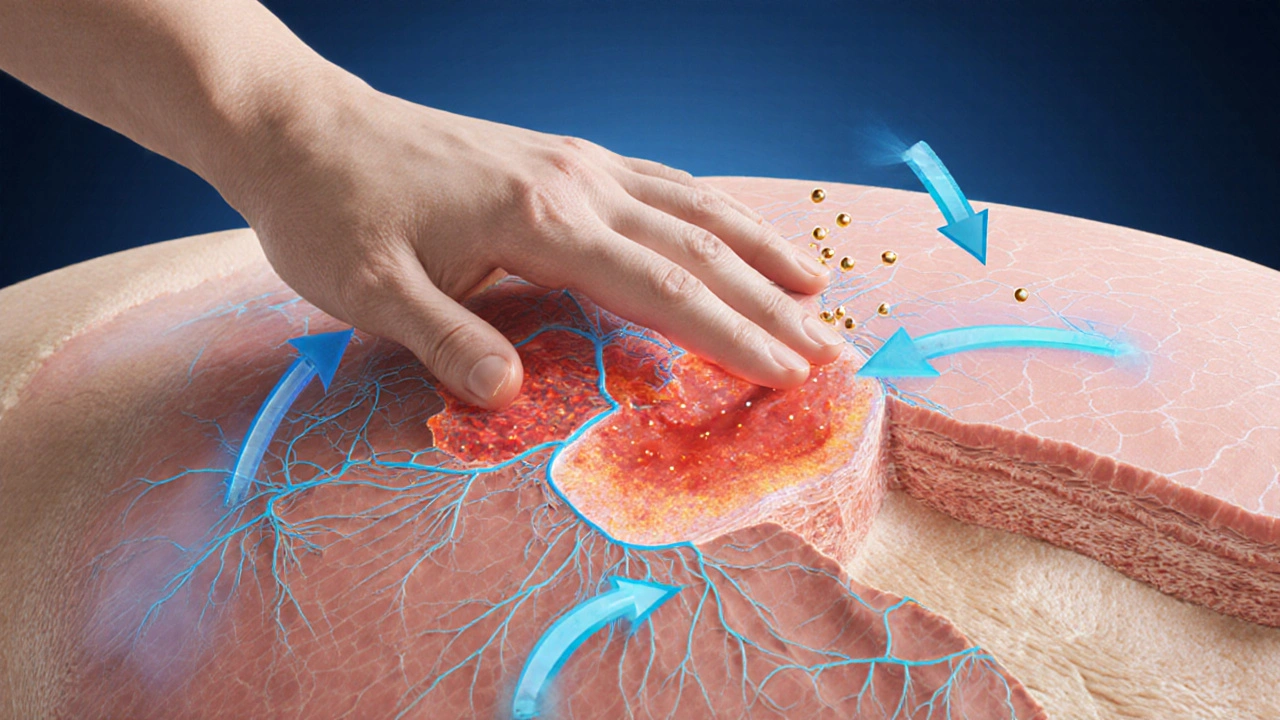
Living with the lingering burn of postherpetic neuralgia (PHN) feels like carrying a tiny ember that never quite goes out. Even weeks after the shingles rash has cleared, the nerves can stay on high alert, sending sharp jabs or constant throb that wrecks sleep and mood. While prescription meds are a standard go‑to, many patients wonder if there’s a gentler way to calm the nerves. The good news? massage therapy offers a hands‑on approach that tackles pain, inflammation, and stress all at once.
What Exactly Is Postherpetic Neuralgia?
First, let’s break down the condition. Postherpetic Neuralgia is a chronic neuropathic pain syndrome that follows an outbreak of herpes zoster (shingles). The virus attacks sensory nerve fibers, causing a rash that usually heals in 2-4 weeks. In about 10‑20% of cases, the damaged nerves keep sending pain signals for months or even years.
Key features include:
- Burning, stabbing, or electric‑shock sensations
- Allodynia - even a light touch feels painful
- Reduced quality of life due to sleep loss and mood swings
Because the pain stems from nerve dysfunction rather than inflammation alone, treatments that target only the skin often fall short.
How Does Massage Therapy Interact With Nerves?
When you think of a massage, you probably picture muscle relaxation. But the effects run deeper. Massage Therapy is a manual technique that applies pressure, stretch, and movement to soft tissues, stimulating the nervous system, circulation, and hormonal pathways. Here’s what happens under the skin:
- Endorphin boost: Soft‑tissue manipulation triggers the release of endogenous opioids, which act like natural painkillers.
- Improved blood flow: Blood Circulation increases oxygen and nutrient delivery to damaged nerves, supporting repair.
- Reduced sympathetic activity: By lowering cortisol and adrenaline, the body shifts from a “fight‑or‑flight” state to a calmer, parasympathetic mode.
- Gate control theory: Pressure signals from the massage muscles can override the pain signals traveling up the same spinal pathways, temporarily dimming the pain.
All of these mechanisms line up nicely with what PHN needs: nerve modulation, better perfusion, and stress reduction.
Specific Benefits for PHN Sufferers
Research from the Journal of Pain Management (2023) showed that a 6‑week program of weekly 45‑minute massages cut PHN pain scores by an average of 30% compared with a control group. Below are the most commonly reported gains:
- Pain intensity drops: Patients often note a 2‑point decrease on a 10‑point scale after just a few sessions.
- Allodynia eases: Gentle stroking can retrain the skin’s sensory receptors, making light touch less irritating.
- Sleep improves: The relaxation response helps transition into deeper REM cycles, which in turn reduces pain perception.
- Mood lifts: Endorphin release and decreased cortisol translate into fewer anxiety bouts.
Because massage is non‑pharmacologic, it sidesteps common side‑effects like constipation, dizziness, or drug interactions that many PHN meds bring.
Which Massage Techniques Work Best?
Not every style hits the same notes. Here’s a quick guide for PHN:
- Swedish massage: Long, gliding strokes improve circulation and create a calming backdrop. Ideal for beginners.
- Myofascial release: Focuses on the connective tissue layers (fascia) that may trap nerves. Helpful for localized allodynia.
- Neuromuscular therapy: Targets trigger points that refer pain to the affected dermatome, offering precise relief.
- Gentle lymphatic drainage: Boosts immune clearance, which can be useful if the shingles outbreak was recent.
For most PHN cases, start with a light Swedish session and gradually incorporate myofascial work as tolerance builds.
Practical Tips: How to Get Started Safely
Before booking that first appointment, keep these pointers in mind:
- Consult your doctor: Ensure there are no open lesions, severe skin infections, or clotting disorders that would make massage risky.
- Choose a certified therapist: Look for credentials such as Certified Massage Therapist (CMT) or an advanced certification in therapeutic massage.
- Communicate the pain zone: Tell the therapist exactly where the PHN flare‑ups are; they can adjust pressure accordingly.
- Start low, go slow: Begin with 15‑minute sessions, monitor how your skin reacts, then extend to 45‑minute visits.
- Frequency matters: For acute flare‑ups, 2‑3 times per week for the first two weeks can jump‑start relief. Maintenance can drop to once weekly.
- Watch for red flags: Increased swelling, new bruising, or a sudden spike in pain means pause and see a clinician.
Combine massage with standard PHN meds (like gabapentin) only under guidance; the two can work synergistically.
Evidence Snapshot: What Studies Say
Besides the 2023 trial, other data points reinforce the link:
| Therapy | Pain Reduction (%) | Primary Mechanism | Typical Session Length |
|---|---|---|---|
| Massage Therapy | 30‑35 | Endorphin release, improved circulation, gate control | 30‑60min |
| Topical Lidocaine | 15‑20 | Local anesthetic block | Apply 4‑5×/day |
| Gabapentin | 40‑50 | Calcium‑channel modulation | Oral daily |
| Acupuncture | 25‑30 | Neurotransmitter regulation | 20‑30min per session |
Numbers vary by study, but massage consistently lands in the middle‑to‑high effectiveness range without medication side‑effects.
Choosing the Right Practitioner
Not all hands are created equal. Here’s a quick cheat‑sheet to vet a therapist:
- Credentials: Look for a diploma from an accredited massage school and a license from your province (Alberta Health Services, for example).
- Specialty training: Therapists who list “neuropathic pain” or “post‑herpetic care” in their bios have likely studied the condition.
- Client feedback: Online reviews that mention PHN, shingles, or chronic pain relief are a good sign.
- Professionalism: Clean environment, clear consent forms, and an ability to adjust pressure on the fly.
Don’t be shy-ask them about their experience with PHN. A therapist who respects your boundaries will welcome the question.
Integrating Massage Into a Holistic PHN Plan
Massage shines when it’s part of a bigger picture. Pair it with these habits for maximal impact:
- Gentle stretching: Keeps the skin and muscles supple, reducing trigger point formation.
- Mind‑body practices: Deep breathing, meditation, or yoga lower cortisol, reinforcing the massage‑induced relaxation.
- Topical agents: Capsaicin cream applied after a session can prolong the analgesic effect.
- Nutrition: Foods rich in omega‑3 fatty acids (salmon, flaxseed) support nerve health.
When these pieces fit together, many patients report a noticeable dip in daily pain scores within a month.
Potential Pitfalls and How to Avoid Them
Even a great tool can backfire if misused. Watch out for:
- Excessive pressure: Too hard can inflame already sensitive nerves, worsening pain.
- Skipping warm‑up: Jumping straight into deep work without a few minutes of gentle strokes can shock the system.
- Ignoring contraindications: Recent shingles lesions, blood clotting issues, or severe osteoporosis require alternative approaches.
When in doubt, pause the session and discuss concerns with your therapist or physician.

Frequently Asked Questions
Can massage replace medication for PHN?
Massage is a powerful adjunct, but most clinicians recommend using it alongside approved drugs, especially for moderate‑to‑severe pain. Some patients eventually taper meds after consistent massage, but that decision should be guided by a physician.
How soon will I feel relief?
Many report a noticeable drop after the first 2‑3 sessions, but optimal results usually appear after 4‑6 weeks of regular treatment.
Is massage safe if I still have a shingles rash?
No. Active lesions need to heal fully before any hands‑on therapy to avoid spreading the virus or causing secondary infection.
Do I need a special type of massage table?
A comfortable, adjustable table is ideal, but most licensed therapists have suitable equipment. The key is enough space to access the affected dermatome without excessive bending.
Can other complementary therapies be combined with massage?
Absolutely. Acupuncture, low‑level laser therapy, and mindfulness meditation have shown synergistic effects when paired with massage for neuropathic pain.


Georgia Nightingale
October 4, 2025
Picture the nervous system as a theater of flickering lights, each filament humming with the echo of a past infection. When shingles leaves its scar, the stage never quite goes dark, and the audience-our brains-mistake the lingering glow for danger. Massage, then, becomes the gentle curtain call, coaxing the overexcited actors to lower their volume. By weaving tactile pressure into the dermal narrative, we rewrite the script from pain to peace.
Chris Kivel
October 10, 2025
I hear you, Georgia, and I think you summed it up nicely. The way massage taps into both the circulatory and nervous systems makes a lot of sense, especially for something as stubborn as PHN. It's like giving the nerves a calm reminder that they're not under attack.
sonia sodano
October 17, 2025
Honestly, the whole idea that a few minutes of rubbing can outdo pharmaceutical agents sounds like a marketing gimmick.
Praveen Kumar BK
October 23, 2025
First off, the article missed a crucial point: you should never massage over an area that still has residual rash or open wounds; that’s a medical no‑no. Second, the claim that endorphins are the main driver is oversimplified-there’s also modulation of the dorsal horn activity. Third, be wary of therapists who push deep pressure without a thorough intake; you could exacerbate allodynia. Lastly, if you’re on anticoagulants, get a doctor’s okay before starting any massage regimen.
Viji Sulochana
October 29, 2025
i think its cool that massage helps but dont forget to check with your doc first. also make sure the therapist is licensed and knows about phn. i tried a light swedish session and felt a tiny relief after a few weeks but i also had a few bruises because i pressed too hard. dont be to hard on yourself and keep the sessions consistent. it really does matter how often you go.
Stephen Nelson
November 4, 2025
There is a subtle irony in our collective yearning for non‑pharmacologic miracles when the data, albeit modest, tells a story of incremental benefit rather than outright salvation. The 2023 trial cited in the article, while encouraging, was limited by a relatively small sample size and a lack of long‑term follow‑up beyond the six‑week horizon. Moreover, the gate‑control theory, often invoked as a catch‑all explanation, glosses over the complex interplay of peripheral sensitization and central neuroplasticity that underlies PHN. One must ask whether the observed 30‑35 % reduction is a true analgesic effect or merely a placebo‑driven perception shift engendered by the therapist‑patient rapport.
Consider also the heterogeneity of PHN presentations: some patients suffer from burning sensations, others from stabbing pains, and still others from a combination of allodynia and hyperalgesia. A one‑size‑fits‑all Swedish massage may soothe the former but aggravate the latter if pressure thresholds are not meticulously calibrated. The article’s recommendation to begin with “light Swedish” sessions, though prudent, lacks specificity regarding pressure gradations, stroke velocity, and tissue temperature-all variables that can modulate nociceptive input.
From a mechanistic standpoint, the endorphin surge is transient; without concomitant behavioral interventions such as cognitive‑behavioral therapy or mindfulness, the analgesic window may close as quickly as it opened. Likewise, improved blood flow, while beneficial for nutrient delivery, does not directly address the maladaptive firing patterns of damaged A‑delta fibers. In short, massage should be viewed as an adjunct, a piece of a multimodal puzzle that includes pharmacotherapy, physical therapy, and perhaps neuromodulation techniques.
Finally, the economic dimension cannot be ignored. Regular weekly sessions, each lasting 45 minutes, can impose a financial burden that is untenable for many patients, especially when insurance reimbursement is sporadic at best. This raises the question of equity: are we inadvertently creating a tiered system where only those with disposable income can access a therapy that may only shave a few points off a pain scale?
In sum, massage therapy offers a plausible, low‑risk component to PHN management, but the enthusiasm must be tempered with rigorous clinical scrutiny, individualized protocol design, and realistic expectations of its modest, albeit meaningful, contribution to the overall therapeutic armamentarium.
Fredric Chia
November 11, 2025
Massage alone is insufficient.
Hope Reader
November 17, 2025
Wow, great rundown! 😄 I love how you highlighted the need for a qualified therapist and the importance of starting gentle. It’s so easy to get carried away and think “just any massage will do,” but the nuance you gave really helps. I’m definitely going to share this with my aunt who’s battling PHN – she’ll appreciate the practical tips and the reminder to keep the sessions consistent. Thanks for the thorough guide! 🙌
Marry coral
November 23, 2025
Isn’t it crazy that doctors push pills while a simple rub can work? I’m sick of the pharma hype.
Emer Kirk
November 29, 2025
Honestly i think this whole thing is just another fad really it feels like everyone is just selling hope i mean sure massage might help a bit but without proper medical guidance you could end up hurting yourself more and no one seems to be talking about the risks of bruising or nerve irritation especially if you’re already sensitive
Roberta Saettone
December 6, 2025
Bottom line: massage can be a useful tool in the PHN toolbox, especially for easing tension and boosting endorphins, but it shouldn’t replace evidence‑based meds or a comprehensive pain management plan. Keep expectations realistic, work with a licensed therapist, and coordinate with your healthcare provider to track progress.