When your liver gets damaged over time-whether from alcohol, fatty liver disease, or hepatitis-the blood flow through it gets blocked. This forces blood to find other paths, increasing pressure in the portal vein. That’s portal hypertension. It’s not a disease on its own, but a dangerous consequence of liver damage that leads to bleeding, fluid buildup, and brain fog. About 9 out of 10 cases come from cirrhosis, and once it develops, it doesn’t go away. The goal isn’t to cure it-it’s to stop the disasters it causes.
What Happens When Pressure Rises
Normal portal vein pressure sits between 5 and 10 mmHg. When it climbs past 10 mmHg-or when the hepatic venous pressure gradient (HVPG) hits 5 mmHg or higher-you’ve crossed into portal hypertension. But it’s not just a number. That extra pressure tears open veins in your esophagus and stomach. These are called varices. They’re like overinflated balloons filled with blood, and they can burst without warning.At the same time, fluid leaks into your belly. That’s ascites. Your liver stops making enough albumin, a protein that keeps fluid in your blood vessels. Without it, fluid pools in your abdomen. You might gain 10 pounds overnight. Your belly swells. Breathing gets hard. Walking becomes a chore. And your kidneys start to fail because your body thinks it’s drowning.
The root problem? Scar tissue. When liver cells die, they’re replaced with stiff fibrous tissue. Blood can’t flow through easily. To make up for it, your body opens up new blood vessels in the gut, flooding the portal system. Nitric oxide spreads through your system, relaxing blood vessels everywhere. That sounds good-but it makes the pressure worse. It’s a vicious loop.
Varices: The Silent Time Bomb
Half of all people with cirrhosis develop varices within 10 years. And 1 in 5 of those will bleed. Once you bleed once, your chance of bleeding again within a year jumps to 60% if you don’t get treatment.Doctors don’t wait for bleeding to happen. They screen with endoscopy. If they see medium or large varices, they don’t just watch. They tie them off with rubber bands-endoscopic band ligation. It’s done in an outpatient setting. One session reduces your bleeding risk by more than half. After that, you take a beta-blocker like propranolol. The goal? Lower your heart rate by 25%. That’s not random. Studies show that’s the sweet spot for cutting bleeding risk by 45% compared to no treatment.
But beta-blockers have a dark side. Many people feel tired, dizzy, or depressed. Some can’t even climb stairs without gasping. On patient forums, people say it feels like your body is running on low battery. That’s why doctors don’t just hand out prescriptions. They adjust doses slowly. They check your blood pressure. They watch for signs your heart can’t handle it.
If you do bleed, it’s an emergency. You’re rushed to the hospital. You get antibiotics right away-usually ceftriaxone-to prevent deadly infections. You get a drug like terlipressin or octreotide to squeeze the blood vessels shut. Then, within 12 hours, you’re on the endoscopy table. Band ligation is done. If it’s a massive bleed, you might need a TIPS procedure.
Ascites: The Swelling That Steals Your Life
Six out of 10 people with cirrhosis will develop ascites. It’s one of the clearest signs your liver is failing. The first step is simple: cut salt. No more than 2,000 mg a day. That means no processed food, no canned soup, no soy sauce. It’s harder than it sounds.Then come the diuretics. Spironolactone is the first-line drug. It blocks aldosterone, a hormone that makes your kidneys hold onto salt and water. You start with 100 mg a day. If that’s not enough, they add furosemide-40 mg a day. Together, they pull fluid out. For most people, this works. 95% of cases respond well.
But when your belly is so swollen you can’t eat or breathe, you need a paracentesis. A needle is inserted into your abdomen to drain the fluid. You might lose 5 liters in one session. That’s like emptying a large soda bottle. But here’s the catch: every liter you remove, you need 8 grams of albumin to replace it. Otherwise, your blood pressure crashes. Your kidneys shut down. That’s why this isn’t done in a clinic-it’s done in a hospital, under supervision.
Some people need this every few weeks. One patient on a liver forum said, “It feels like a tire iron is stuck in my abdomen.” After three sessions in two months, she quit her job as a nurse. She couldn’t stand for more than 20 minutes.
When diuretics and paracentesis stop working, you have refractory ascites. That’s when TIPS comes in. A small metal mesh tube is threaded through a vein in your neck, down into your liver, and across to the main vein leading to your heart. It creates a shortcut for blood, lowering pressure in the portal system. Success rate? 90-95%. But 1 in 4 people develop hepatic encephalopathy-brain fog, confusion, even coma-within a year. It’s a trade-off: less fluid, but your brain might not work right.

Non-Cirrhotic Portal Hypertension: A Different Beast
About 1 in 10 cases of portal hypertension isn’t from cirrhosis. This is called non-cirrhotic portal hypertension (NCPH). It can come from portal vein clots, schistosomiasis, or rare genetic conditions. The treatment is totally different.If it’s caused by a clot, you don’t take beta-blockers. You take blood thinners. Warfarin or direct oral anticoagulants. The goal? Keep your INR between 2 and 3. That’s the range where clots dissolve without causing dangerous bleeding. One study showed that patients on anticoagulants had a 70% lower chance of the clot spreading.
But here’s the problem: most doctors aren’t trained to spot NCPH. It’s often missed. If you have portal hypertension but no signs of cirrhosis-normal liver enzymes, no history of heavy drinking-you need a specialist. A biopsy or elastography might be needed to rule out early scarring.
The New Tools: What’s Changing in 2025
The field is changing fast. Five years ago, the only way to measure portal pressure was HVPG-a catheter inserted through the neck or liver. It’s invasive. Risky. Expensive. Only 45% of U.S. hospitals do it regularly. But now, there’s a new option: spleen stiffness measurement.Using a device like FibroScan, doctors can measure how stiff your spleen is. A stiff spleen means high portal pressure. Studies show it’s 85% accurate. That’s almost as good as HVPG. In Europe, many centers now use it to screen patients instead of doing catheter tests.
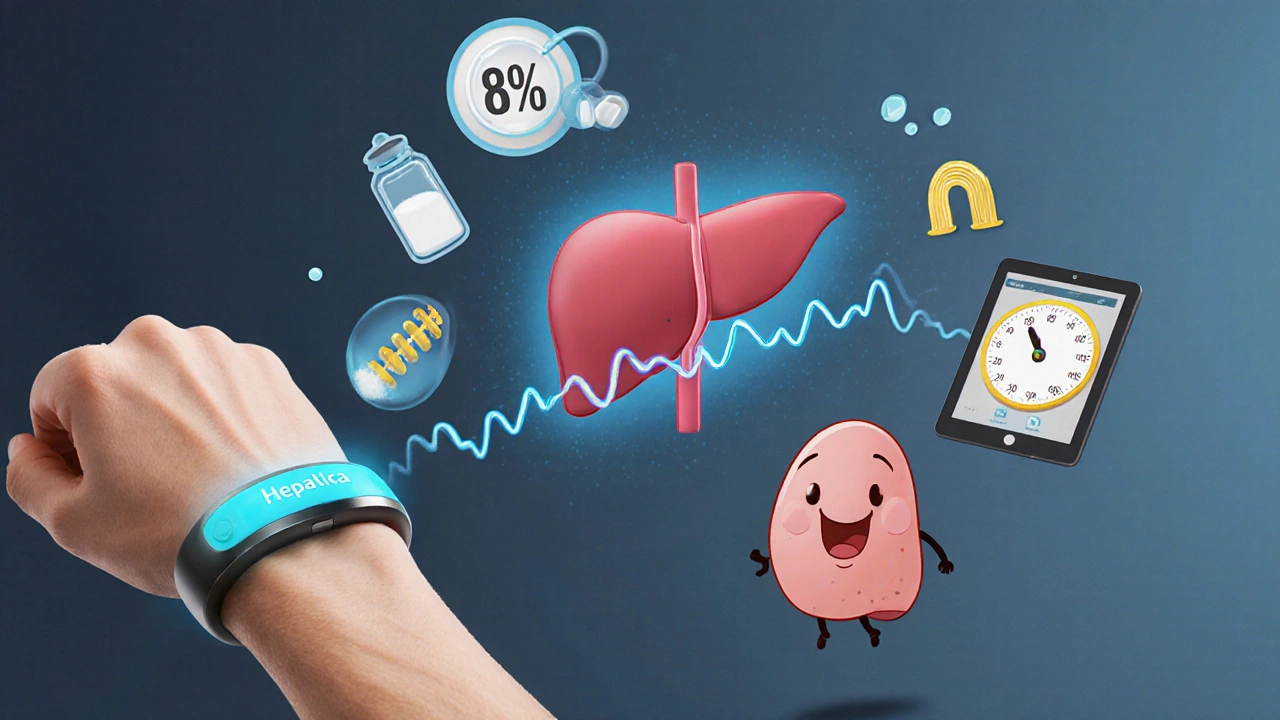
And then there’s the Hepatica SmartBand. Approved by the EMA in September 2023, it’s a wearable device that estimates portal pressure using bioimpedance. No needles. No hospital. Just wear it for 10 minutes. It’s not perfect-82% accuracy-but for monitoring over time? Game-changing.
Drug trials are also heating up. Simtuzumab, a new antibody, showed a 35% drop in HVPG in non-cirrhotic patients. It’s not approved yet, but it’s in phase 3. And AI? Mayo Clinic built a model that predicts variceal bleeding with 92% accuracy. It uses your age, platelet count, spleen size, and albumin level. No endoscopy needed.
What’s Not Working
Despite all the advances, the death rate from variceal bleeding hasn’t dropped in 30 years. It’s still 15-20% within six weeks of a bleed. Why? Because we treat the pressure, not the body’s response. Dr. Patrick Northup says we’re ignoring the whole system: your heart, your blood vessels, your kidneys. You can lower portal pressure, but if your heart can’t pump enough blood, you still crash.And liver transplant? It’s the only real cure. But the wait in the U.S. is 14 months on average. For someone with recurrent bleeding and ascites, that’s a long time to survive.
Living With It
People with portal hypertension don’t just need meds. They need structure. A low-salt diet. Daily weight checks. A phone call to the doctor if they gain 2 pounds in 2 days. A plan for what to do if they vomit blood.One man on Reddit, age 52, said: “I live with the fear every morning. Did I sleep okay? Did I wake up with blood in my mouth? Is today the day?” That’s the emotional toll. It’s not just physical. It’s anxiety, isolation, depression.
Quality of life scores for these patients are 35-40 points lower than healthy people their age. That’s like being 20 years older. But those who get TIPS or consistent banding? They report feeling like they got their life back. One woman said, “After my TIPS, I cooked Thanksgiving dinner for the first time in three years.”
The key isn’t just medicine. It’s awareness. It’s follow-up. It’s knowing when to call 911.
What is the main cause of portal hypertension?
Cirrhosis is the cause in about 90% of cases. It’s the scarring of the liver that blocks blood flow, forcing pressure to build up in the portal vein. The remaining 10% are due to non-cirrhotic causes like portal vein clots, infections, or rare genetic disorders.
Can portal hypertension be cured?
No, not yet. Portal hypertension is a consequence of liver damage, and once scarring sets in, it’s permanent. Treatment focuses on managing complications-like stopping bleeding from varices or draining ascites-rather than reversing the pressure. Liver transplant is the only cure, but it’s not always possible.
How do you know if you have varices?
You won’t feel them until they bleed. That’s why screening is critical. If you have cirrhosis, you should have an endoscopy every 1-2 years to check for varices. If none are found, you may only need screening every 2 years. If medium or large varices are found, treatment starts immediately.
Is ascites always a sign of advanced liver disease?
Yes. Ascites usually appears when cirrhosis is moderate to severe. It’s one of the key markers doctors use to stage liver disease. If you develop ascites, your 5-year survival drops significantly without treatment. But with proper management-diuretics, salt control, and sometimes TIPS-many people live for years with it.
What’s the difference between propranolol and nadolol for portal hypertension?
Both are non-selective beta-blockers used to lower portal pressure. Propranolol is more commonly used because it’s cheaper and has more long-term data. Nadolol lasts longer and is taken once daily, which can improve adherence. Studies show they work equally well for preventing bleeding. The choice often comes down to side effects and cost.
Can you drink alcohol with portal hypertension?
Absolutely not. Alcohol accelerates liver damage and increases portal pressure. Even small amounts can trigger bleeding or worsen ascites. If you have portal hypertension, you must stop drinking completely. This isn’t optional-it’s life-or-death.
How often do you need to get an HVPG test?
HVPG isn’t done routinely. It’s used when treatment response is unclear or when considering TIPS. After starting beta-blockers, a repeat HVPG may be done after 1-3 months to see if pressure dropped by at least 20% or below 12 mmHg. That’s the target for preventing rebleeding. For most people, non-invasive tests like spleen stiffness are used instead.
What happens if you miss a dose of your beta-blocker?
Missing one dose won’t cause immediate bleeding, but it increases your risk over time. Beta-blockers work by keeping portal pressure low. If you skip doses, pressure can rebound. If you miss a dose, take it as soon as you remember-but never double up. If you miss more than two days in a row, call your doctor. You may need to restart slowly to avoid sudden blood pressure drops.


Saket Sharma
November 18, 2025
Varices are a ticking time bomb-band ligation isn't optional, it's survival. Beta-blockers? Half the patients quit because they feel like zombies. But skipping them? That's how you end up in the ER with a mouth full of blood. No drama. Just facts.
Alex Boozan
November 18, 2025
Let’s be clear-this isn’t medicine, it’s triage. The system’s broken. We’re patching leaks while the whole damn house burns. TIPS? Great. But why are we waiting until someone’s drowning to fix the plumbing? American healthcare prioritizes profit over prevention. End of story.
mithun mohanta
November 19, 2025
Did you know? Portal hypertension isn’t even ‘real’ in the classical sense-it’s a *syndrome*, a cascade, a systemic collapse! And yet, we treat it like a single disease?! Beta-blockers? Diuretics? Band ligation? All Band-Aids on a ruptured aorta! We need to reframe the entire paradigm-*hepatic hemodynamics*, *endothelial dysfunction*, *nitric oxide dysregulation*-this isn’t just cirrhosis, it’s a *systemic vascular catastrophe*!!!
Evan Brady
November 20, 2025
For anyone reading this and scared: you’re not alone. I’ve been managing this for 7 years. The salt restriction? Brutal. The beta-blockers? Made me feel like I was walking through syrup. But after TIPS? I hiked the Grand Canyon last spring. It’s not a cure-but it’s a second life. Don’t give up. Find a good hepatologist. Track your weight daily. And yes, even if you hate it-take your pills.
Ram tech
November 21, 2025
why do docs even bother with endoscopy? just give the beta blockers and call it a day. i mean, who has time for all that? also, i heard the new smartband thing is fake. like, totally. its just a fancy watch. they dont even know how it works. lol
Jenny Lee
November 23, 2025
One woman cooked Thanksgiving after TIPS. That’s the whole story right there.
Erica Lundy
November 25, 2025
There is a profound metaphysical tension here: we treat the vessel, not the vessel's origin. Portal hypertension is not merely a hemodynamic phenomenon-it is the somatic manifestation of a body’s surrender to chronic insult. The liver, once a silent architect of homeostasis, becomes a monument to neglect. And we, in our hubris, deploy bandages, beta-blockers, and shunts-technological palliatives-as if the soul of the organ could be repaired by mechanical intervention. Is this medicine-or merely the ritual of deferred despair?
Kevin Jones
November 26, 2025
They say cirrhosis is the #1 cause. Bullshit. It’s alcohol, greed, and denial. People keep drinking. Corporations keep selling. Doctors keep prescribing Band-Aids. And then we’re shocked when someone bleeds out in a waiting room? Wake up. This isn’t a medical crisis-it’s a moral one.
Premanka Goswami
November 28, 2025
Ever wonder why the HVPG test is so rare? Because Big Pharma doesn’t want you measuring pressure-they want you on lifelong drugs. The spleen stiffness scan? It’s a Trojan horse. The FDA is in bed with the catheter companies. They don’t want cheap, accurate diagnostics. They want recurring revenue. And don’t get me started on the ‘Hepatica SmartBand’-it’s a surveillance tool disguised as a medical device. Your vitals are being sold to insurers. You’re being tracked. You’re not a patient-you’re a data point.
Alexis Paredes Gallego
November 29, 2025
Let me guess-the article was written by a hepatologist who’s never met a patient who actually lived with this. You talk about TIPS like it’s magic. But 25% get encephalopathy? That’s not a trade-off-that’s a prison sentence. And who’s paying for the 14-month transplant wait? The uninsured? The underinsured? The ones who can’t take time off work? This isn’t medicine. It’s a lottery. And you’re holding the losing ticket.
Shravan Jain
November 30, 2025
Propranolol? 25% HR reduction? That’s the gold standard? Pathetic. The real issue is the gut-liver axis. Endotoxemia. Bacterial translocation. The portal system isn’t just under pressure-it’s poisoned. And yet, we ignore the microbiome. We ignore inflammation. We ignore the fact that cirrhosis isn’t just scarring-it’s immunological collapse. Band ligation won’t fix that. You need to treat the *source*, not the symptom. But of course, that’s too complex for a 15-minute consult.
Brandon Lowi
December 1, 2025
They call it portal hypertension-but it’s really the body screaming. Every varice, every liter of ascites, every confused thought-it’s the liver’s last roar before the silence. We treat it like a plumbing issue. But it’s not. It’s a soul in slow-motion collapse. And we hand out diuretics like candy. Meanwhile, the real cure-abstinence, justice, dignity, community-isn’t even on the table. We don’t need more gadgets. We need to stop letting people drown in neglect.