FDA Generics: What They Are, Why They Matter, and What You Need to Know
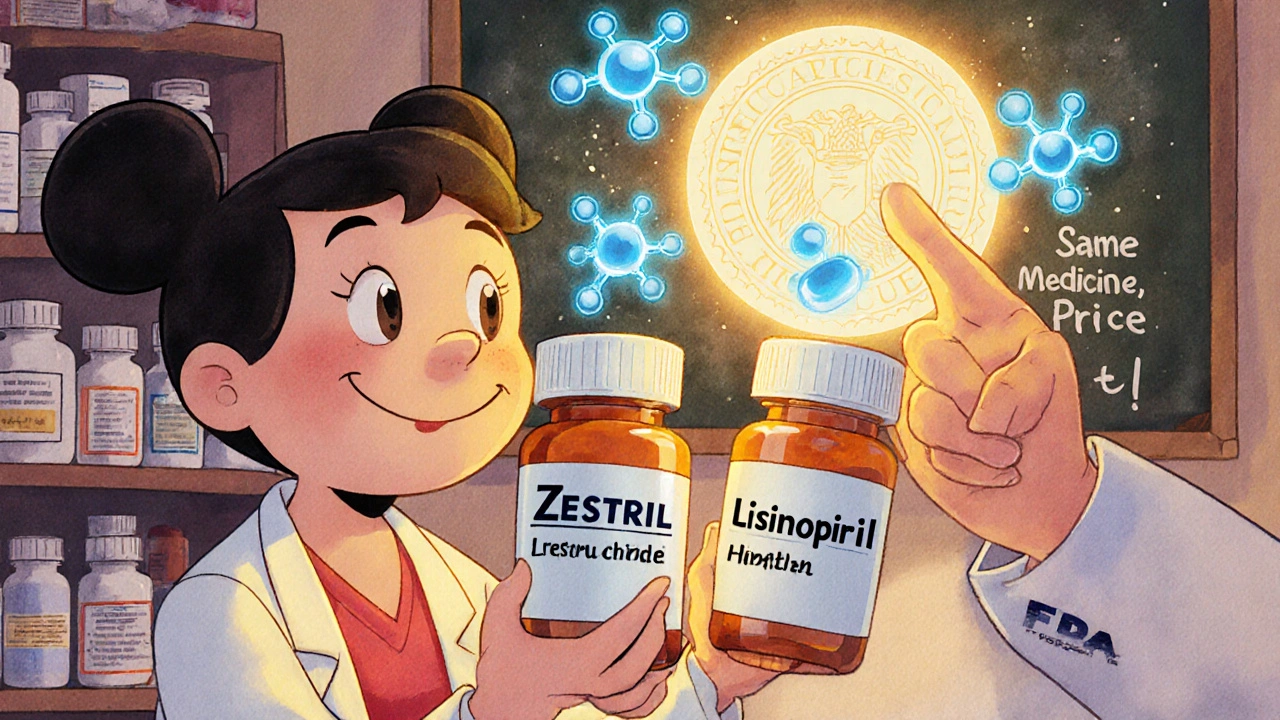
When you hear FDA generics, drug versions approved by the U.S. Food and Drug Administration to match brand-name medications in safety, strength, and performance. Also known as generic medications, they’re not cheap knockoffs—they’re scientifically identical to the originals, often costing 80% less. Every year, the FDA approves hundreds of these drugs, and the savings add up to billions in healthcare costs. You might not realize it, but chances are you’ve taken one this month—whether it was metformin for diabetes, lisinopril for blood pressure, or naproxen for pain.
The real trick isn’t just that generics work—they do—but how hard it is to get them approved. For simple pills, the process is straightforward: prove they release the same amount of active ingredient at the same rate as the brand. But for complex generics, drugs like inhalers, creams, or injectables that rely on delivery systems, not just chemistry, proving they’re the same becomes a scientific maze. A cream might look identical, but if it doesn’t penetrate skin the same way, it won’t work the same. That’s why some generics take years to clear FDA review, and why some never make it to market at all.
And here’s something most people don’t talk about: physician liability, the legal risk doctors face when prescribing generics because generic manufacturers can’t be sued for side effects. If a patient has a bad reaction, the blame often lands on the prescriber, not the maker. That’s why some doctors stick to brand names—not because they think they’re better, but because they’re trying to protect themselves. Meanwhile, the drug savings, the billions saved annually thanks to FDA-approved generics replacing expensive brands keep climbing. In 2022 alone, generics saved U.S. patients over $370 billion. That’s not just a number—it’s someone’s insulin, their blood pressure pill, their painkiller they can actually afford.
But not all generics are created equal. Some are made in factories with poor oversight. Others get approved based on flawed testing. That’s why you’ll find posts here about bioequivalence—how scientists test whether a generic really behaves like the original in your body. You’ll also see how restarting a medication after a break can be deadly if you don’t adjust the dose, even if it’s just a generic version. And you’ll learn why some people on kidney meds need to watch creatine supplements, or why anticholinergic drugs linked to dementia might be hiding in plain sight—even in generic form.
This isn’t just about saving money. It’s about understanding what you’re taking, who’s responsible when things go wrong, and how the system works behind the label. Whether you’re a patient trying to stretch your budget, a caregiver managing multiple meds, or a healthcare worker navigating legal gray zones, the truth about FDA generics affects you. Below, you’ll find real, no-fluff guides on how these drugs are tested, how they impact your health, and what you should ask your doctor before you pick up that prescription.