Peripheral Artery Disease: Causes, Risks, and Medications That Help
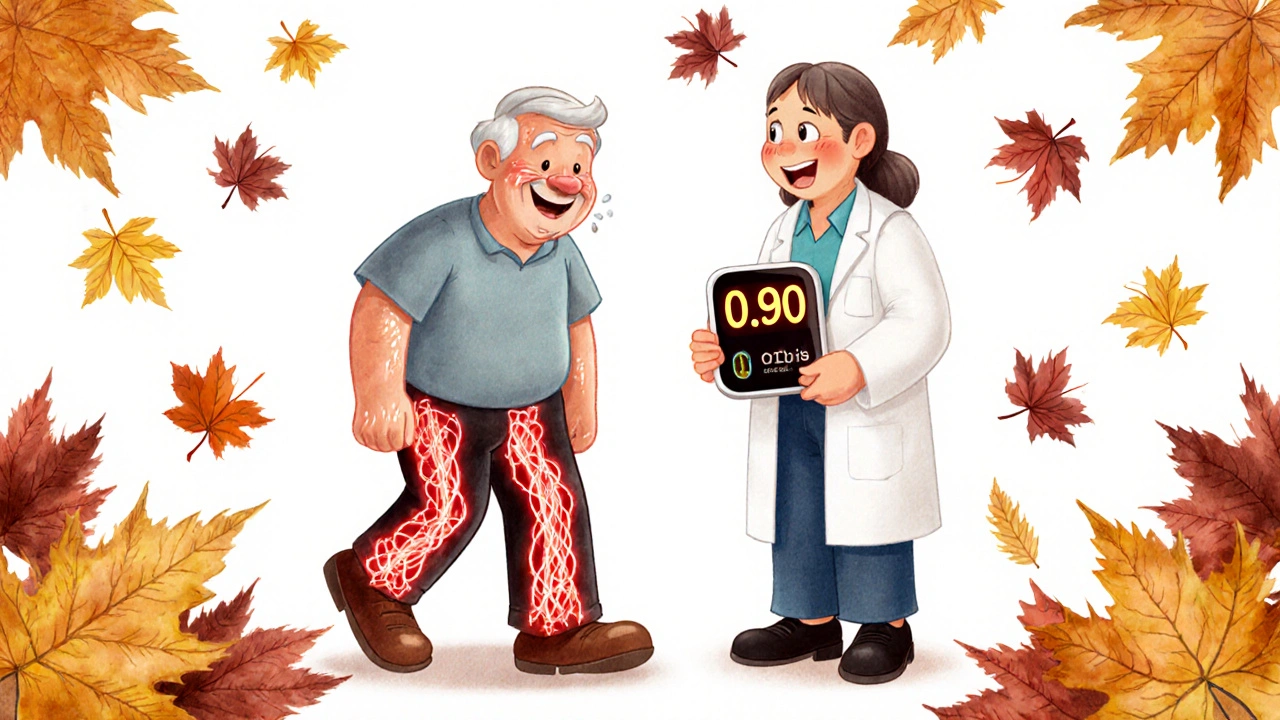
When your arteries narrow and block blood flow to your legs, arms, or other body parts, you're dealing with peripheral artery disease, a condition where plaque builds up in the arteries outside the heart and brain, limiting circulation. Also known as PAD, it's not just a leg problem—it's a warning sign your whole vascular system is under stress. Many people ignore early symptoms like leg pain when walking, thinking it’s just aging or being out of shape. But PAD is often linked to deeper issues like atherosclerosis, the hardening and narrowing of arteries due to fatty deposits, which also drives heart attacks and strokes. If you have PAD, you’re far more likely to have blockages elsewhere too.
It doesn’t show up out of nowhere. diabetes, a condition that damages blood vessels over time and impairs healing is one of the biggest risk factors. So is hypertension, high blood pressure that wears down artery walls. Smoking, high cholesterol, and being over 50 also pile on the risk. You might not feel pain until the blockage is serious—so if you’ve got any of those conditions, don’t wait for symptoms to get worse. Early testing can catch PAD before it leads to amputation or heart trouble.
Medications don’t fix the blockage, but they stop it from getting worse. Statins lower cholesterol and stabilize plaque. Blood pressure drugs like ACE inhibitors reduce strain on arteries. Antiplatelets like aspirin or clopidogrel keep clots from forming. Some people need more aggressive treatment—stents, angioplasty, or even surgery—but for most, the right combo of meds and lifestyle changes can keep them walking without pain. The posts below break down exactly which drugs work, how they interact with other conditions like kidney disease or diabetes, and what to watch out for when combining treatments. You’ll find real-world advice on managing PAD alongside other chronic issues, avoiding dangerous drug overlaps, and understanding why some meds help more than others.