Tolerance Loss: What It Is, Why It Happens, and How It Affects Your Medications
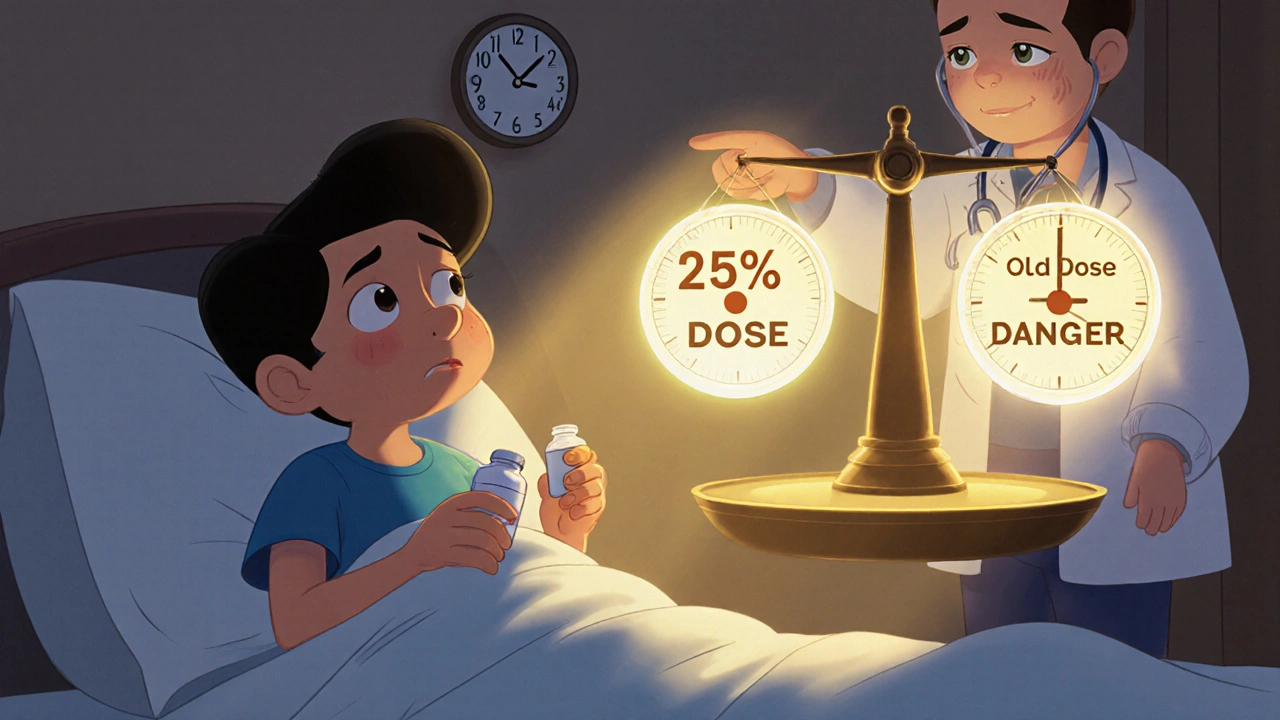
When your body stops responding to a medication the way it used to, you’re experiencing tolerance loss, a condition where the body’s response to a drug diminishes over time, requiring higher doses for the same effect. This isn’t just about needing more pills—it’s your system adapting in ways that can quietly mess with your health. It’s not the same as addiction, but it often shows up alongside it, especially with painkillers, antidepressants, or sleep aids. You might notice your headache relief fading, your anxiety creeping back, or your sleep getting worse—even though you’re taking the same dose.
Tolerance loss doesn’t happen in a vacuum. It’s closely tied to drug interactions, when one medication changes how another works in your body. For example, if you’re on an anticholinergic like dicyclomine for cramps, and you start taking something else that affects your nervous system, your body’s ability to respond to either drug can shift. That’s why withdrawal symptoms, the physical or mental reactions when you reduce or stop a drug your body has adapted to often appear not just when you quit, but when you switch meds or add new ones. Even something as simple as drinking coffee with your thyroid pill can throw off how your body processes it, leading to unexpected tolerance changes.
It’s also why medication effectiveness, how well a drug does what it’s supposed to do in your body isn’t just about the dose. Your liver, your gut bacteria, your kidney function—all of it plays a role. If you’re taking creatine and monitoring kidney health, or using protonix for acid reflux while also on blood pressure meds, your body’s handling of each drug can shift over time. That’s tolerance loss in action: not because you’re taking too much, but because your system is changing.
Some people think tolerance loss means they’re weak or doing something wrong. It’s not. It’s biology. Your body is trying to stay balanced, and sometimes that means it stops responding the way it did at first. The problem isn’t you—it’s that most doctors don’t talk about this until things go sideways. That’s why you’ll find real stories here: how people managed tolerance with antispasmodics, why some stopped feeling the effects of their pain meds, how changing diet or adding probiotics quietly altered their drug response, and what to do when your meds just don’t feel the same anymore.
Below, you’ll see real cases where tolerance loss showed up in unexpected places—from thyroid pills and caffeine to kidney meds and antidepressants. No fluff. Just what works, what doesn’t, and what to watch for before it’s too late.