Opioid Constipation Prevention Guide
Opioids can cause constipation in nearly everyone after a few weeks of use. This tool helps you plan for constipation prevention based on your treatment timeline. Start prevention early to avoid complications.
Important Safety Note
Do not stop opioids abruptly. Always consult your doctor before changing medication. This tool provides general guidance only.
When you're dealing with severe pain - after surgery, from cancer, or due to a major injury - opioids can be a lifeline. But for every person who finds relief, many more face a different kind of struggle: the side effects. Constipation, drowsiness, and nausea aren't just minor inconveniences. They're common, predictable, and often long-lasting problems that can make taking these medications feel worse than the pain itself.
Constipation: The One Side Effect That Never Goes Away
If you're on opioids long-term, constipation is almost guaranteed. Studies show it affects nearly everyone who uses these drugs for more than a few weeks. Unlike drowsiness or nausea, which often fade as your body adjusts, constipation sticks around. That’s because opioids don’t just block pain signals in your brain - they also slow down your gut. Opioids bind to receptors in your intestines, making the muscles there less active. Food moves slower. Water gets sucked out of your stool. The result? Hard, painful bowel movements that feel impossible to pass. Many patients report going days without a bowel movement, and some end up needing enemas or hospital visits because it got so bad. The key is not to wait until it happens. The American Academy of Family Physicians recommends starting a laxative regimen the same day you start your opioid. Don’t wait for discomfort. Don’t hope it’ll be fine. Use a combination of a stimulant laxative like senna and an osmotic agent like polyethylene glycol. These work together - one wakes up your gut, the other pulls water in to soften stool. For those who still struggle, there are targeted options like methylnaltrexone (Relistor) or naloxegol (Movantik). These drugs block opioid effects in the gut without touching the pain relief in your brain. They’re not cheap, but for people who can’t function because of constipation, they can be life-changing.Drowsiness: When Your Brain Feels Like It’s Underwater
The first few days on opioids? You might feel like you’re moving through molasses. That’s drowsiness - a normal, expected side effect. Between 20% and 60% of people experience it when they start. Your mind feels foggy. Concentration fades. You nod off during conversations or while watching TV. Most people adjust within a week or two. Their bodies build a tolerance. But for 10% to 15% of long-term users, the fog never fully lifts. That’s when it becomes dangerous. Driving, operating machinery, even walking up stairs becomes risky. For older adults or those with existing cognitive issues, the mental fog can be mistaken for dementia. The solution isn’t always to stop the opioid. Sometimes, it’s about timing. Take your dose at night if you can. Avoid scheduling important tasks right after dosing. Talk to your doctor about reducing the dose slightly - even a 10% drop can make a big difference in alertness without losing pain control. In rare cases, doctors may consider stimulants like methylphenidate (Ritalin) to counteract the drowsiness. But there’s little solid evidence they work well for opioid-induced fatigue, and they come with their own risks - increased heart rate, anxiety, insomnia. Use them only if everything else fails, and only under close supervision.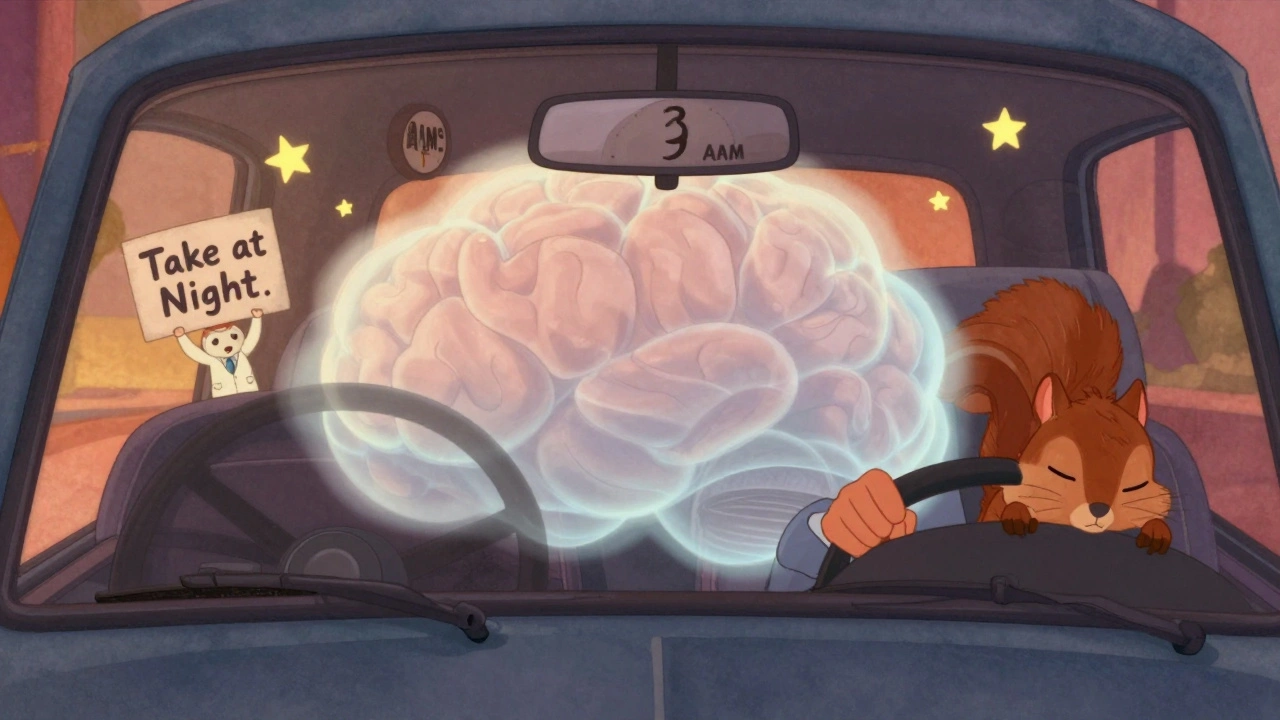
Nausea: Why Your Stomach Feels Like It’s in Revolt
Nausea hits about one in four people when they start opioids. It’s not just an upset stomach - it’s a full-body reaction. Your brain’s vomiting center gets triggered directly by the drug. Your stomach empties slower. You feel queasy, sweaty, and sometimes vomit. The good news? Most people get over it within a week. Your body adapts. But for 1 in 10, the nausea lingers. That’s when it starts to break your will to keep taking your medicine. You skip doses. You stop altogether. Your pain comes back worse. Treatment depends on what’s causing it. If it’s your brain’s vomiting center being overstimulated, dopamine blockers like metoclopramide or prochlorperazine help. If your stomach is just sitting still, drugs like ondansetron (Zofran), which block serotonin, are more effective. Sometimes, an antihistamine like promethazine works best - it calms both nausea and drowsiness. Don’t just take one pill and give up. Try one class for 3-4 days. If it doesn’t help, switch. Many patients need to go through two or three different anti-nausea drugs before finding the right fit.Why These Side Effects Matter More Than You Think
These aren’t just annoying symptoms. They’re the reason many people stop taking opioids - even when they still need them. And that’s dangerous. The CDC reports that over 8 million Americans misused prescription opioids in 2023. More than two-thirds of them said they did it to relieve physical pain. That’s not drug-seeking behavior. That’s people trying to manage pain when the side effects of their prescribed meds make life unbearable. Worse, if you suddenly quit opioids because you can’t handle the nausea or constipation, you risk withdrawal. That means intense vomiting, diarrhea, sweating, anxiety - and yes, your pain can spike higher than before. The FDA warns that abrupt discontinuation can lead to serious harm, including suicide risk. The goal isn’t to avoid opioids entirely. It’s to use them safely. That means preparing for side effects before they start. It means talking to your doctor about constipation before your first pill. It means having a plan for drowsiness before you get behind the wheel. It means knowing which anti-nausea drug to try if the first one fails.
What You Can Do Right Now
- If you’ve just started opioids: Ask your doctor for a laxative prescription today. Don’t wait for constipation to happen.
- If you’re feeling drowsy: Avoid driving or operating heavy machinery for the first week. Take your dose at bedtime if possible.
- If you’re nauseous: Keep a log. Note when it happens, how bad it is, and what you’ve tried. Bring it to your next appointment.
- If you’re thinking of stopping: Don’t quit cold turkey. Talk to your doctor about tapering slowly. Withdrawal can make pain worse.
- If you’re on multiple medications: Review everything with your doctor. Some drugs - like benzodiazepines or alcohol - make drowsiness and breathing problems much worse.
What’s Next for Opioid Therapy
Newer drugs are being developed to separate pain relief from side effects. One type, called peripherally-acting mu-opioid receptor antagonists (PAMORAs), targets only the gut - fixing constipation without affecting pain control. Others aim to activate pain-blocking pathways in the brain while avoiding the ones that cause nausea or drowsiness. But until those become widely available, the best tool we have is awareness. Know what to expect. Plan ahead. Don’t suffer in silence. Your doctor can’t help you if you don’t tell them what’s wrong. Opioids aren’t perfect. But for many, they’re still the best option for managing severe pain. The difference between success and failure often comes down to how well you manage the side effects - not the pain itself.Is constipation from opioids permanent?
No, constipation from opioids isn’t permanent, but it usually lasts as long as you’re taking the medication. Unlike drowsiness or nausea, which often improve with time, constipation typically doesn’t go away on its own. That’s why doctors recommend starting laxatives right away - not waiting until you’re struggling to go.
Can I drive if I feel drowsy from opioids?
No. Feeling drowsy from opioids impairs reaction time and decision-making just like alcohol. Most people adjust within a week or two, but until you know how the drug affects you, avoid driving, operating machinery, or making important decisions. If drowsiness lasts longer than two weeks, talk to your doctor about adjusting your dose or timing.
Why does nausea happen with opioids?
Opioids trigger nausea in two ways: they directly stimulate the vomiting center in your brainstem, and they slow down your stomach’s emptying. This combination makes you feel queasy. The effect is strongest when you first start taking them, but for some people, it lasts longer. Different anti-nausea drugs target different pathways, so you may need to try a few before finding one that works.
Should I stop opioids if side effects are too bad?
Don’t stop suddenly. Quitting opioids cold turkey can cause severe withdrawal - including vomiting, diarrhea, sweating, and intense pain. Instead, talk to your doctor. They can help you adjust your dose, add medications to manage side effects, or slowly taper off if needed. Stopping abruptly can make your pain worse and increase the risk of turning to unsafe sources for relief.
Are there alternatives to opioids for pain?
Yes. Depending on your condition, options include physical therapy, nerve blocks, non-opioid pain relievers like acetaminophen or NSAIDs, antidepressants for nerve pain, or even procedures like spinal cord stimulation. Many pain specialists now use a multimodal approach - combining several treatments to reduce or eliminate the need for opioids. Always ask your doctor what else might work for your specific situation.


Robert Altmannshofer
December 4, 2025
Been on opioids for two years post-surgery. Constipation was brutal at first-like trying to push a bowling ball through a straw. Started senna + MiraLAX on day one, and it made all the difference. No more ER trips. No more crying in the bathroom. Just… regular. People don’t talk about this enough. It’s not weakness. It’s physiology. Treat it like part of the treatment plan.
Also, drowsiness? Totally real. Took my dose at 8 PM instead of 10 AM. Suddenly I could watch my kid’s soccer games without nodding off. Small change. Huge quality of life boost.
vanessa parapar
December 5, 2025
Ugh, I hate when people act like constipation is some mysterious side effect. It’s literally in the damn pamphlet. If you didn’t plan for it, you’re not being responsible. Start laxatives day one. End of story. Also, don’t blame the drug for your poor lifestyle. Drink water. Eat fiber. Move your butt. Literally.
And no, Zofran isn’t magic. Try promethazine first. It’s cheaper and knocks out nausea AND sleepiness. Stop overcomplicating things.
Ben Wood
December 6, 2025
Let’s be real-this whole opioid narrative is a pharmaceutical industry construct. They know constipation is inevitable, so they sell you Relistor for $2,000 a month. Meanwhile, the FDA and CDC are all like, ‘Just take laxatives!’ like we’re all just… lazy? No. It’s systemic. The system doesn’t care if you’re functional. It cares if you’re compliant.
And don’t get me started on ‘drowsiness is temporary.’ My uncle’s been on oxycodone for 11 years. He still can’t read a book without falling asleep. They call it ‘tolerance.’ I call it chemical imprisonment.
Melania Dellavega
December 7, 2025
I’ve sat with people who’ve been on these drugs for years. Not because they want to, but because the pain won’t let them go. And the side effects? They’re not just physical. They’re lonely. You can’t go out. You can’t focus. You feel like a burden. I’ve seen people cry because they couldn’t hold their grandchild without falling asleep.
It’s not about willpower. It’s about dignity. If we’re going to give people this level of relief, we owe them the tools to live with it-not just survive it.
And yes, the laxatives work. But so does compassion. Someone needs to ask, ‘How are you really doing?’-not just, ‘Are you taking your meds?’
Sakthi s
December 9, 2025
Start laxatives early. Simple. Works. No drama.
gladys morante
December 9, 2025
I don’t trust any of this. The government and pharma are hiding something. Why do they push opioids so hard? Why aren’t they talking about the real cause of chronic pain? It’s not the injury-it’s the toxins in our food, the EMFs, the fluoride. They want you dependent. They profit from your suffering. I stopped everything cold. Now I drink celery juice and meditate. My pain? Gone. Not because of drugs. Because I woke up.
Abhi Yadav
December 10, 2025
Life is pain. Opioids just make you aware of it. The body is a temple, but the mind? The mind is a prison. When the gut slows, it’s not constipation-it’s the soul refusing to move. You think you’re fighting nausea? You’re fighting the weight of existence.
Try yoga. Or fasting. Or chanting. The pills are just a bandage on a wound that never healed.
🙂
Julia Jakob
December 11, 2025
They say ‘start laxatives day one’ like it’s that easy. What if you’re on Medicaid and the only thing they cover is Dulcolax? And it doesn’t work? And your doctor won’t prescribe MiraLAX because ‘it’s not FDA approved for this’? Yeah, real helpful.
And don’t even get me started on the ER nurses who treat you like a junkie when you ask for help with constipation. Like you’re asking for heroin. You’re asking for a bowel movement. I’ve cried in waiting rooms over this. Not because I’m weak. Because the system is broken.
Kathleen Koopman
December 13, 2025
Just wanted to say thank you for this post. I’ve been on opioids for 8 months after my spinal fusion. Constipation was the worst part. Tried everything. Then my PT told me to try a Squatty Potty. 🤯 I was skeptical. But now? I go daily. No laxatives needed. Just posture. Who knew? Also, the drowsiness faded after 10 days. Still take it at night. And I use a weighted blanket. It helps me sleep AND feel less anxious. 🙏
Nancy M
December 13, 2025
In India, we have a traditional remedy for opioid-induced constipation: flaxseed soaked overnight in water, then blended with warm milk and honey. Works better than most OTC laxatives, and it’s cheap. My cousin used it after her knee surgery-no hospital visits, no prescriptions. Just food as medicine.
Also, in Tamil Nadu, they use ginger tea with black salt for nausea. Not science-y, but it’s been passed down for generations. Maybe we’re missing something in our over-medicalized approach.
Not saying ditch the science. Just… maybe blend it?
Shannon Wright
December 14, 2025
As someone who’s spent 15 years in palliative care, I’ve watched hundreds of patients navigate this exact struggle. What I’ve learned: the side effects aren’t just medical-they’re existential. Constipation makes you feel trapped in your own body. Drowsiness steals your moments with loved ones. Nausea makes food, once a comfort, feel like a threat.
We treat these as ‘manageable’ because we don’t know how else to cope. But they’re not manageable-they’re devastating. And yet, we don’t talk about the grief that comes with it. The grief for the life you had before the pain. The grief for the life you can’t have while on the meds.
So yes, use senna. Yes, take it at night. Yes, try Zofran. But also-sit with the person. Hold their hand. Ask them what they miss. Because sometimes, the most powerful medicine isn’t in the pill bottle. It’s in the quiet presence of someone who sees the whole person, not just the symptoms.
Robert Asel
December 15, 2025
It is a well-documented, peer-reviewed, evidence-based fact that opioid-induced constipation (OIC) affects 85-95% of long-term users, as per the Journal of Pain and Symptom Management, 2021. Furthermore, the American College of Gastroenterology explicitly recommends combination therapy with stimulant and osmotic laxatives as first-line management. Any deviation from this protocol constitutes substandard care. Additionally, the use of non-pharmacological interventions such as ‘squatty potties’ is not supported by Level 1 evidence and should be discouraged in clinical practice. This post, while well-intentioned, risks promoting anecdotal and unvalidated practices that could compromise patient safety.
Rachel Nimmons
December 16, 2025
Did you know the FDA approved Relistor in 2008… right after the opioid crisis started getting media attention? Coincidence? I don’t think so. They knew people would get addicted to the painkillers… so they made a $500/month pill to fix the side effect so people would keep taking them. It’s not medicine. It’s a trap. And they’re selling it to you as ‘care.’