Medication Safety and Generic Drugs in November 2025: Key Guides and Insights
When it comes to generic drugs, pharmaceutical products that contain the same active ingredients as brand-name drugs but are often much cheaper. Also known as non-brand medications, they make up over 90% of prescriptions filled in the U.S. Yet many people still doubt their effectiveness—not because of science, but because of perception. This month’s collection dives deep into why that gap exists, how it affects your health, and what you can do about it.
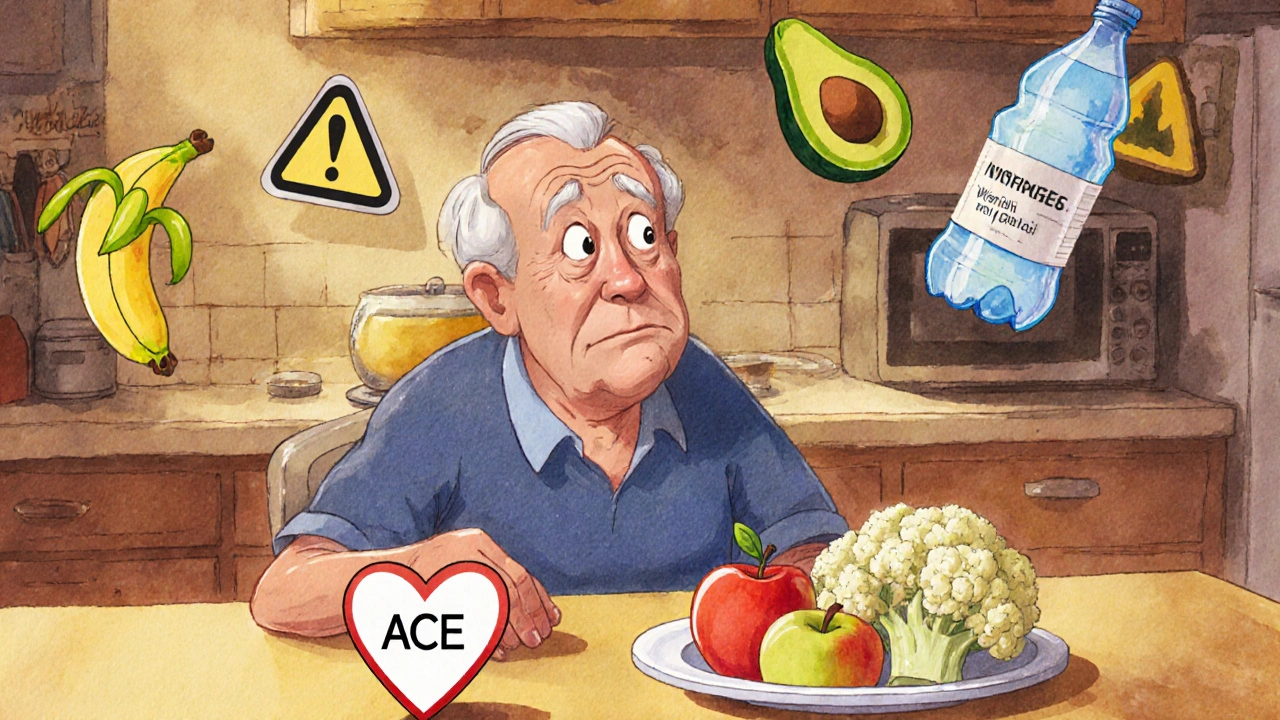
One of the biggest concerns around medications is safety—especially when you’re restarting a drug after a break, managing chronic conditions, or using multiple prescriptions at once. Naloxone nasal spray, a life-saving medication that reverses opioid overdoses within minutes. Also known as Narcan, it’s now available without a prescription in most places, and this month’s guide shows exactly how to use it—no medical training needed. But naloxone isn’t the only urgent topic. ACE inhibitors, common blood pressure drugs that can raise potassium levels dangerously if not managed. Also known as angiotensin-converting enzyme blockers, they’re often prescribed for heart failure and kidney disease, but pairing them with high-potassium foods like bananas or spinach without monitoring can lead to hyperkalemia—a condition that can stop your heart. That’s why we broke down exactly which foods to limit, how often to test your blood, and what newer treatments can help you stay safe.
Another major theme this month was the hidden complexity behind everyday medications. For example, if you’re taking creatine, a popular supplement for muscle growth and energy. Also known as creatine monohydrate, it raises creatinine levels in blood tests, which can falsely look like kidney damage—especially if you’re also on kidney disease medications, drugs like ACE inhibitors or diuretics that affect how your body processes waste. Also known as renal protective agents, they’re meant to protect your kidneys, but combining them with creatine without proper testing can lead to unnecessary panic or even wrong treatment decisions. We showed you how to tell real kidney trouble from a lab glitch.
And then there’s the issue of drug interactions. Antispasmodics like dicyclomine, often used for IBS, can clash with common antidepressants, antihistamines, and even some heart medications, causing confusion, dry mouth, or urinary retention. We mapped out the most dangerous combos and gave you safer alternatives. Same with SIBO—bacterial overgrowth in the small intestine—where breath tests are widely used but often misleading. We explained why a positive result doesn’t always mean you need antibiotics, and what diet changes actually work long-term.
This isn’t just theory. These are real problems people face every day: someone restarting an opioid after a hospital stay, a diabetic choosing between Glycomet SR and Ozempic, a senior on five meds wondering why they feel foggy. The articles this month give you the tools to ask better questions, spot red flags, and take control—not just of your meds, but of your health outcomes.
Below, you’ll find 17 detailed, no-fluff guides that cut through the noise. Whether you’re managing a chronic condition, helping a loved one through an overdose, or just trying to understand why your generic pill feels different, these posts give you what you need—straight, clear, and ready to use.